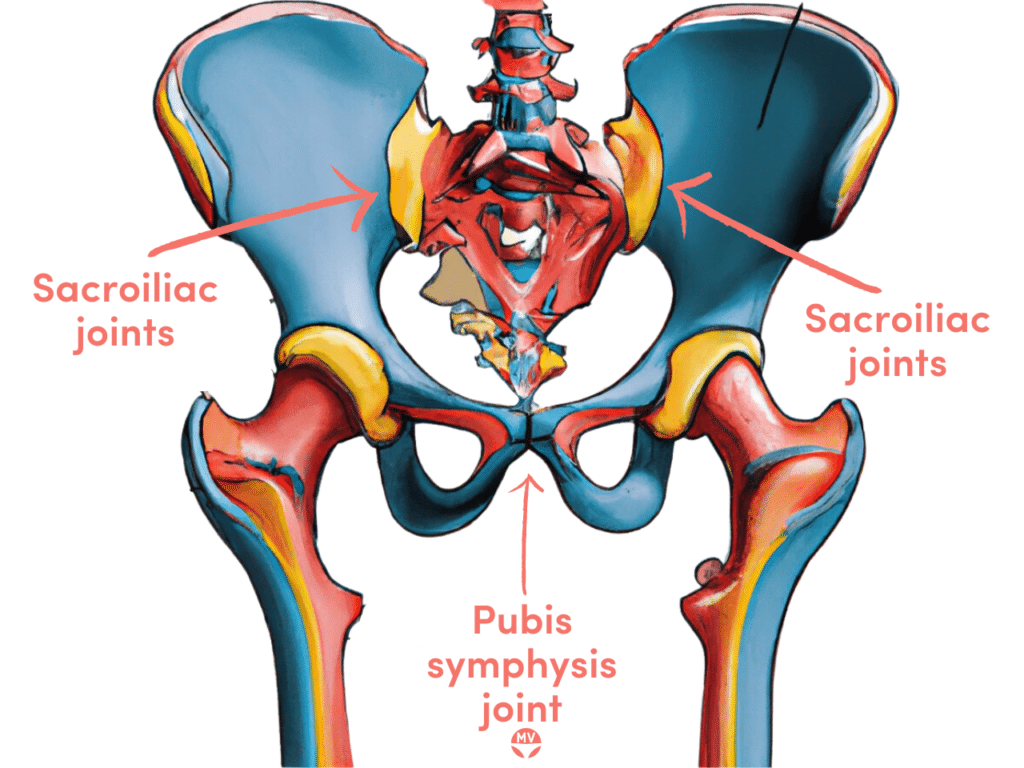
Osteitis pubis is characterised by pain and inflammation of the pubis symphysis joint.
Inflammation of the pubic symphysis joint is typically caused by repetitive damage known as ‘shearing’ from surgery, accidents, one leg longer than the other, or biomechanical foot or shoe issues.
Muscle issues, inflexibility, sacroiliac (SI) joint dysfunction or joint misalignment can cause atypical shearing forces that initiate and aggravate microtrauma, causing inflammation, pain and muscle spasms.
Causes of osteitis pubis
Pregnancy can be a major contributing factor, alongside pelvic surgeries or major physical traumas. Repeated minor trauma, such as from sports or exercise, and sometimes rheumatological drivers, can cause osteitis pubis.
Contributing factors to osteitis pubis include running on concrete, going from zero to hero with a new exercise routine, wearing poorly fitting shoes, movement disturbances and stiff muscles, but everyone is different in their biomechanics and body and must be assessed individually by an experienced professional.
Symptoms of osteitis pubis
- Lower pelvic pain and aching – groin, hip, bladder, clitoris, vagina, perineum, scrotum, testicles
- Painful sex (dyspareunia)
- Pain worse for coughing, sneezing, sitting, standing, lying on one side, changing direction in movement, kicking, pivoting on one leg, running or jumping
- Clicking or popping when walking or during vigorous movement
- Loss of groin region flexibility
- Pain may be a dull ache, sharp stabbing, tenderness to the touch
- May occur during pregnancy due to joint pressure and relaxin release (known as symphysis pubis dysfunction (SPD)), which softens ligaments
- May worsen after birth or pelvic surgery
- May contribute to pelvic floor muscle dysfunction
Diagnosing osteitis pubis
Per a healthcare practitioner’s recommendations, X-ray, CT or other scans are suitable for visualising and diagnosing osteitis pubis. Irregularity and widening of the pubic symphysis are the key findings.
Spinal, pelvic and lower limb biomechanics should be evaluated to assess misalignments and muscle or ligament tension or laxity.
Differential diagnoses include pubic symphysis separation/dysfunction (SPD), hernia or groin strain.
Treating osteitis pubis
Joint realignment and mobilisation are key to realigning the sacroiliac and pubic symphysis joints. Therapies for inflammation and pain will likely be employed, alongside rebalancing, stability exercises, and movement re-education. Pelvic support belts may be used.
Anti-inflammatories, stretching and strengthening exercises are used. Novel treatments are being developed, but no standard exists to treat osteitis pubis. Surgery may be used as a last resort in severe cases, but the success rate is low and further problems are not uncommon from the surgery.
The pubic symphysis joint may also be called the pubis symphysis, symphysis pubis or symphysis pubica joint.
Specially formulated probiotic for vaginal application to promote a healthy vaginal microbiome.
Unique, comprehensive BV, AV and 'mystery bad vag' treatment guide, one-of-a-kind system, with effective, innovative treatments.





