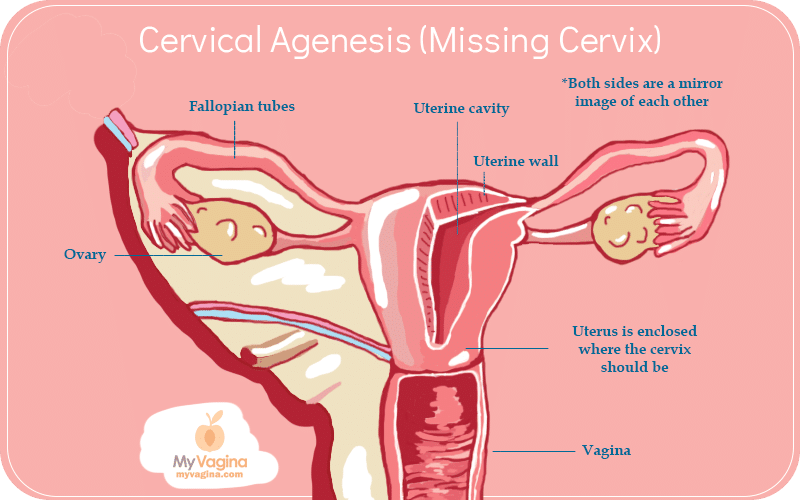
Cervical agenesis is a congenital condition whereby the foetus does not develop a cervix, the connecting ‘neck’ between the uterus and vagina.
There are other variations including cervical atresia or cervical dysgenesis, where the cervix does exist, but is improperly formed and not functional. Cervical agenesis occurs in about one in every 80,000 live female births.
This condition often comes with vaginal abnormalities, with about half of all women with cervical agenesis having a normal and functioning vagina, with the rest having vaginal hypoplasia, which is a short or nonexistent vagina. The vagina may end in a blind pouch.
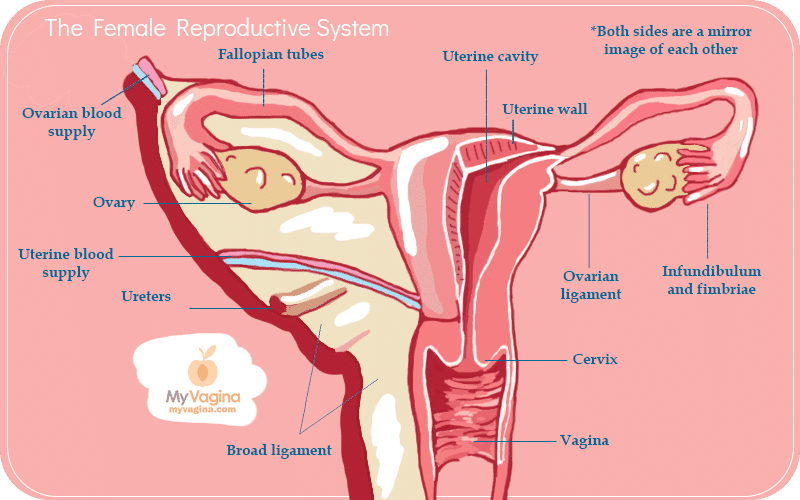
A normal cervix
Cervical agenesis
Diagnosis of cervical agenesis
Teenage girls may present to a doctor because they haven’t started their period (primary amenorrhoea), but are getting pelvic pain. This pain is due to a build-up of menstrual blood that has no escape (hematocolpos), so builds up in the uterus, causing pain due to the pressure build-up.
This blood would normally travel through the cervix and out the vagina. Imaging tests will be done to establish what structures exist, perhaps a combination of MRIs and ultrasounds.
Why does cervical agenesis happen?
Cervical agenesis is an interruption of the growing foetus whereby the paramesonephric duct doesn’t form into the cervix as it is supposed to.
Treatment and management of cervical agenesis
The first port of call is usually to put the teenager on the pill (combined oral contraceptive), synthetic progesterone (progestin called medroxyprogesterone acetate), or a special drug that acts on the pituitary gland (gonadotropin-releasing hormone agonist) which suppresses menstruation and relieves the pain.
Surgical options include the complete removal of the uterus (hysterectomy) to totally avoid the bleeding problem. Other solutions have been to join the vagina and uterus together (uterovaginal anastomosis), or to create a new canal that can act as a cervix, though at the moment, outcomes are not great for the latter options.
The operation is called a neovaginoplasty. The major issues here are infections and other issues that are generally avoided when one has a functioning cervix: that is, protection from uterine, fallopian tube and ovarian infection, foreign bodies, and protective mucous production.
These options are imperfect, but pregnancy has been reported in women with cervical agenesis who have had surgery.
Untreated cervical agenesis will eventually lead to other conditions due to the build-up of menstrual blood – hematocolpos, hematosalpinx, endometriosis, endometrioma, and pelvic adhesions.
Specially formulated probiotic for vaginal application to promote a healthy vaginal microbiome.
Unique, comprehensive BV, AV and 'mystery bad vag' treatment guide, one-of-a-kind system, with effective, innovative treatments.





