If you have severe pain with your period, you might have endometriosis. Endometriosis has been a recognised issue for several hundred years, but diagnosis and research into this inflammatory condition didn’t start in earnest until much more recently.
Some new research areas provide insights into how naturopaths can support those with endometriosis, to improve fertility and reduce painful symptoms.
Endometriosis: severe pain, slow to diagnose
A 2019 Australian government report says a whopping one in nine women are diagnosed with endometriosis by age 40-44. This statistic means you almost certainly know someone with endometriosis – even if they don’t know it yet.
Women with endometriosis make up about 1.5% of hospitalisations in that age bracket – endometriosis is everywhere and can affect someone dramatically.
In my clinical practice, I see women ages 16-46 seeking help with endometriosis. They want a reduction in pain or are looking to get pregnant soon.
Those with endometriosis can take a long time to be diagnosed – an average of 6.5 years, with an invasive laparoscopic surgery to identify the condition.
Period pain can be very painful for some of us, even without endometriosis, but most women with endometriosis suffer for a long time, thinking their pain is normal and that periods are just painful. The ‘deal with it’ mentality that we’re conditioned into by society. Period pain has been normalised.
My previous blog post on the types of period pain that are normal explains what is considered severe, so if you think you might have endometriosis, please read this post.
But remember, pain levels do not always indicate how extensive your endometriosis is.
Supporting women with endometriosis using new research
We’re still not 100% clear on what causes or worsens endometriosis – why do some women get it and some don’t? Why can some women have endometriosis lesions but not experience painful periods?
Previously, naturopaths have worked towards managing pain and healing tissue in those with endometriosis. But new research has broadened our scope and options for treating endometriosis, which is very exciting.
Point 1: Endometriosis is related to the immune system
Part of this new research has shown that the immune system is deeply connected with endometriosis. Therefore, supporting healthy immunity is one of our primary goals when treating endometriosis.
A Japanese study1 from 2018 found that endometriosis is likely to be an immune system disorder.
While having genetic immune dysfunction is not uncommon, having other triggers can also be a major problem:
- dairy and gluten
- bacteria from the gut move to the pelvis
- food contains nickel
- nutrient-deficient diet results in poor immunity
Supporting the immune system in endometriosis
Removing suspect foods is important – removing possible immune-trigger foods that could be causing the reaction. Dairy and gluten intolerance are the first two problem foods on the list.
I’ve seen so many women with endometriosis get off dairy and it’s made an enormous difference – so I often start there. Many of these women already suspected dairy as a problem food, so they are usually willing to make the necessary changes.
Once a few months have gone by without dairy, and no positive changes have been seen, or if there is a gluten allergy in the family (coeliac disease), gluten-containing foods are next on the list to go. The usual suspects here are bread, cakes, biscuits, pasta, pizza, and burgers.
My immune-supporting nutrients include zinc, N-acetylcysteine, turmeric, berberine and echinacea. I make up each person a unique herbal formula for their particular symptoms and what I consider the underlying features of the person’s endometriosis picture.
Point 2: Endometriosis is worsened by high oestrogen
Some signs of high oestrogen include heavy periods and clotting. The endometrial lining grows thicker under the influence of oestrogen across a menstrual cycle and will cause heavier, more painful periods when someone has endometriosis.
Reducing oestrogen levels is potentially important in some people with endometriosis. I check your symptoms and see if it seems like there is high oestrogen or not, and check any test results.
Reducing oestrogen may include eliminating dairy, reducing foods that are high in histamine, ensuring the bowels are moving, ensuring the liver is working well, and using diet modifications and herbal medicine. I also support the gut microbiome. I might use calcium D-glucarate or encourage greater progesterone levels with herbs to balance oestrogen levels.
Endometriosis symptoms can worsen if a person is in perimenopause – a stage of our lives with naturally less progesterone and relatively higher oestrogen levels. Many other symptoms will also get worse during this time of change.
Those in perimenopause often do well with progesterone support and dropping high histamine foods.
Point 3: Bacteria may cause or contribute to endometriosis
Many studies show that of those with endometriosis, 90% have bowel disturbances (irritable bowel symptoms) and experience regular bouts of constipation or diarrhoea. A diagnosis may have been made of irritable bowel syndrome (IBS) or small intestinal bacterial overgrowth (SIBO).
Problematically, IBS and SIBO symptoms can have a lot in common with endometriosis symptoms – it might be hard to work out which area is causing the pain.
Endometrial lesions may be found in the bowels and even in the rectum/colon, and with every menstrual cycle, pain may be due to endometriosis lesions, not a bowel condition or dietary intolerances.
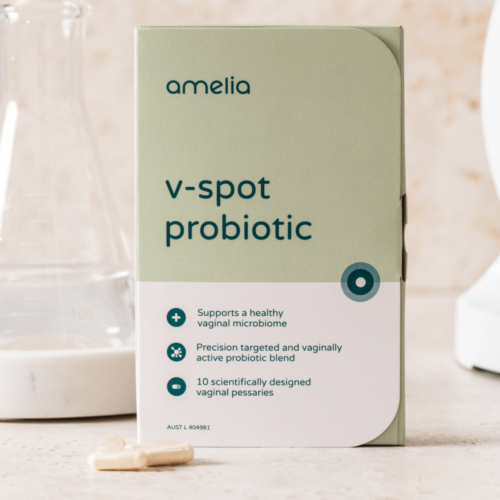
A 2018 study2 found that the menstrual blood of those diagnosed with endometriosis was ‘highly contaminated’ with Escherichia coli (E. coli) – a gut bacteria – than those without endometriosis. The suggestion was that the gut bacteria had translocated from the digestive tract to the pelvis. Lower levels of protective lactobacilli species were also found in the vagina of those with endometriosis.
I support a healthy gut and vaginal microbiome with antimicrobial herbs like berberine and prebiotic foods.
Testing for bacterial or fungal imbalances is an important part of my practice, supporting my clients with endometriosis. I use a GI Map, a comprehensive stool microbiome test for gut dysbiosis, and comprehensive vaginal microbiome testing. After analysing the tests, I choose my herbal medicines, probiotics, and prebiotics and work to improve the microbiome sites and intestinal integrity.
Treating IBS or SIBO is a very important part of my focus with endometriosis clients. Improving bowel movements and balancing bacteria and yeasts can significantly affect overall immune system function and inflammation.
Bacteria as a cause or contributing factor to endometriosis is a very interesting hypothesis, as it brings together my special areas of interest in microbiome testing of the gut and vagina with endometriosis clients.
Point 4: Endometriosis may be related to nickel allergy
In 2015, a study3 demonstrated that nickel allergy is a risk factor for developing endometriosis. This huge study was performed across 11 years on about 5,000 South Korean women. The nickel allergy study is adjacent to endometriosis being an immune system issue.
Nickel is found in metal fixings such as jewellery and belt buckles, but interestingly, also in skin products. One of my important questions for clients is, do you react to jewellery? Then work towards a nickel-free existence as much as possible, including dietary and clothing sources.
What’s next for endometriosis?
I’m hoping that endometriosis will be much better understood very soon. It’s a very difficult experience for women with this condition.
If you think you might have endometriosis, but haven’t been diagnosed yet, visit your doctor, who will refer you to a gynaecologist to be tested.
If you have a diagnosis of endometriosis and want support, please book a consultation with me and we can explore your individual biology and symptoms. I would be delighted to be part of your support team!
References
- 1.Izumi G, Koga K, Takamura M, et al. Involvement of immune cells in the pathogenesis of endometriosis. J Obstet Gynaecol Res. Published online January 5, 2018:191-198. doi:10.1111/jog.13559
- 2.Khan KN, Fujishita A, Hiraki K, et al. Bacterial contamination hypothesis: a new concept in endometriosis. Reprod Med Biol. Published online January 18, 2018:125-133. doi:10.1002/rmb2.12083
- 3.Yuk JS, Shin JS, Shin JY, Oh E, Kim H, Park WI. Nickel Allergy Is a Risk Factor for Endometriosis: An 11-Year Population-Based Nested Case-Control Study. Shankar EM, ed. PLoS ONE. Published online October 6, 2015:e0139388. doi:10.1371/journal.pone.0139388
Specially formulated probiotic for vaginal application to promote a healthy vaginal microbiome.
Unique, comprehensive BV, AV and 'mystery bad vag' treatment guide, one-of-a-kind system, with effective, innovative treatments.