Aerobic vaginitis (AV) and bacterial vaginosis (BV) are two common but very different types of vaginal infections. While they may sometimes share symptoms like discharge and irritation, the causes, diagnosis, and treatments are not the same, and getting the right diagnosis matters.
If you’ve ever been diagnosed with BV but your treatment didn’t work, or your symptoms seemed more inflammatory or painful than expected, you might be dealing with aerobic vaginitis instead.
Here, we’ll help you understand how AV and BV differ, what causes them, and how each condition is treated effectively.
1. How is AV different from BV?
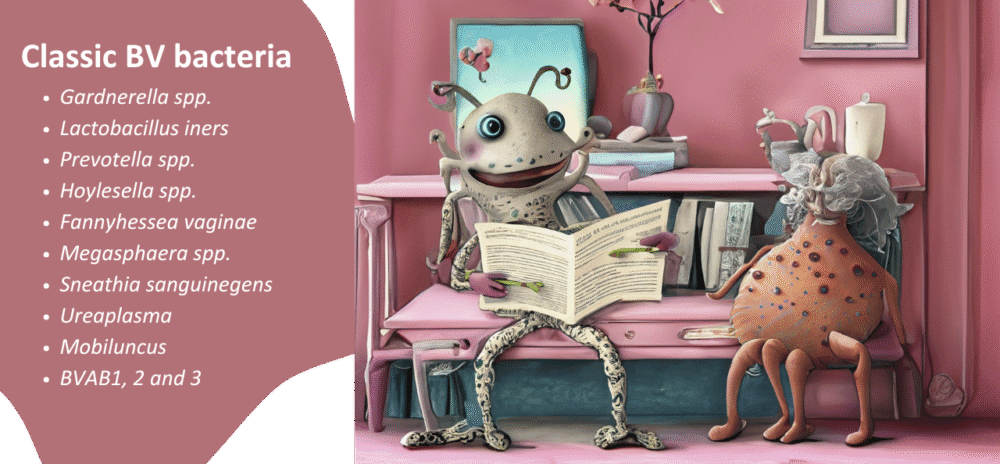
BV is caused by an overgrowth of anaerobic bacteria, like Gardnerella vaginalis, Prevotella, and Megaspheara species, to name a few. These bacteria disrupt the normal balance of the vagina, leading to a drop in protective Lactobacillus species and an increase in vaginal pH.
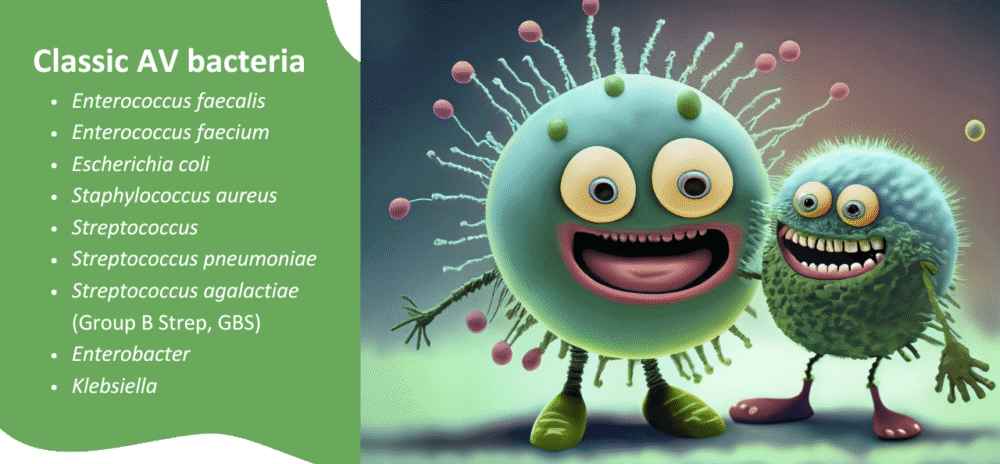
AV, on the other hand, is caused by aerobic bacteria – oxygen-loving microbes – such as Staphylococcus aureus, Escherichia coli, Enterococcus faecalis, and Streptococcus agalactiae. These microbes don’t just disrupt the vaginal flora – they cause inflammation, irritation, and tissue damage. That’s why AV is sometimes referred to as ‘inflammatory vaginosis’.
While both conditions involve a disturbed vaginal ecosystem, AV is more likely to involve immune system activation, epithelial cell damage, and noticeable inflammation. BV often doesn’t cause as much obvious inflammation.
2. What causes aerobic vaginitis?
Aerobic vaginitis is linked to vaginal dysbiosis (an imbalance in microbes), often following antibiotic use, hormonal changes (like low oestrogen), or poor immune response.
HOT TIP!
At the My Vagina specialist clinic, we see a surprising number of people where a male partner has, without warning, switched from anal to vaginal penetration. AV is the result. Educate your sexual partners! Double dipping fingers, toys or penises is NOT on the menu. Wash with hot soapy water and start fresh. While E. coli, Enterococcus, and Streptococcus agalactiae are common gut flora, they can also be commensals or transient colonisers in the lower urogenital tract, particularly postpartum, postmenopause or post-antibiotics.
BV often has few symptoms beyond a fishy odour, whilst AV can be extremely uncomfortable. It can even resemble yeast or thrush, or a sexually transmitted infection.
The key culprit in AV is aerobic bacteria that have found a comfortable home and multiplied in the vagina, often dislodging protective Lactobacillus species. These aerobic bacteria release toxins, disrupt the vaginal mucosa, and trigger inflammation.
3. Aerobic vaginitis symptoms and diagnosis
AV is frequently misdiagnosed as BV, candida (yeast), or vulvovaginal atrophy. If your symptoms include pain, itching, burning, or yellow discharge, and your treatment for BV or yeast hasn’t worked, it may be worth being tested more thoroughly to rule out AV.
Common aerobic vaginitis symptoms include:
- Vaginal burning or irritation
- Symptoms improve during menstrual bleeding
- pH may be normal or high (many AV bacteria are lactic acid-producers)
- Yellow or greenish discharge (often foul-smelling)
- Vaginal dryness or tightness
- Pain during sex
- Redness or swelling of the vulva
- Spotting or bleeding from inflamed tissues
At the doctor, AV is usually diagnosed via vaginal swab and microscopy, but can also be detected via a Next-gen sequencing (NGS) Juno vaginal microbiome test taken at home. Your doctor will look for signs of inflammation, lack of protective Lactobacillus, presence of aerobic bacteria, and immature epithelial cells.
If you’re not sure what’s going on, a more sensitive test is often recommended to clarify which microbes are involved.
4. Is aerobic vaginitis serious?
Yes – aerobic vaginitis can be serious if left untreated. But most often, it is truly uncomfortable, and that is serious because it interrupts your life so much.
Because it involves inflammation and tissue damage, AV can lead to complications like:
- Recurrent infections
- Vaginal wall thinning or ulceration
- Increased risk of STI transmission
- Negative pregnancy outcomes (if pregnant)
- Ongoing discomfort that affects daily life and sexual function
The good news is that aerobic vaginitis is treatable, but the approach needs to be specific. Standard BV treatments, such as metronidazole, are not preferred for treating AV, as other types of antibiotics are more specific and targeted to aerobic microbes.
5. Treatment options for aerobic vaginitis
Successful AV treatment depends on clearing the aerobic bacteria infection, reducing inflammation, and restoring a healthy vaginal microbiome. Standard medical treatment varies between practitioners, with effective antiseptics such as Fluomizin common in Europe.
In most other places, antibiotics such as clindamycin are the only medical treatment offered. However, antibiotic therapy is discouraged where possible due to clindamycin’s often short-lived effect on AV bacteria, and its potential to promote resistance genes for more serious infections, such as methicillin-resistant Staphylococcus aureus (MRSA) and group B streptococci.
Treating AV with non-drug options is considered important, as antibiotic therapy is damaging to the ecosystem in several important ways. Short antibiotic therapy is more useful, with other strategies in play to resolve AV.
At My Vagina, we approach AV with a combination of targeted treatments:
- Aunt Vadge’s AV Rescue blend – a direct antimicrobial blend designed to clear aerobic bacteria infection without disrupting Lactobacillus
- V‑Spot Probiotic – a vaginal probiotic containing Lactobacillus crispatus to support the restoration of protective flora
- Aunt Vadge’s Oral AV Herbal Formula – to support systemic immune modulation and help clear stubborn infections
- Fluomizin (dequalinium chloride) – an antimicrobial agent targeting both BV and AV
- Accurate vaginal pH strips – for at-home tracking of pH, to monitor your progress
All these are part of our recommended AV treatment approach. AV can take several weeks to clear, and the healing phase may be slower than with BV, especially if the vaginal lining is inflamed or damaged, or if other areas of the body are involved, like the gut or mouth microbiome.
If treatment is not getting the results you’re after, schedule a consultation with one of My Vagina’s expert naturopaths. Each appointment includes a thorough health assessment to find the cause of your symptoms and a comprehensive practitioner-only treatment plan.
6. BV symptoms and treatment – what’s the difference?
BV tends to be more subtle in symptoms but frustrating in its recurrence.
Common BV symptoms include:
- Thin, watery, greyish discharge
- Fishy odour, especially after sex
- No itching, pain, or swelling (usually)
BV is diagnosed via symptoms, pH testing, Amsel criteria, Nugent score on microscopy, or with newer PCR/NGS vaginal microbiome testing. Cultures are not typically useful.
BV treatment often includes:
- Fluomizin
- Aunt Vadge’s BV Rescue and Oral BV Herbal Formula (oral and vaginal antimicrobial support)
- Accurate vaginal pH strips
- Life-Space Women’s Microflora Probiotic
- For persistent cases, our Four-Pronged Approach Fixer Boxes
The key difference between AV and BV treatment is that AV requires anti-inflammatory support and restoration of the vaginal lining, while BV is more about rebalancing microbes and breaking down biofilms that protect anaerobic bacteria.
7. Can AV and BV exist at the same time?
Yes – and this can complicate both diagnosis and treatment. Mixed infections involving both anaerobic and aerobic bacteria are increasingly common. In these cases, treatment needs to target both types of microbes.
Aunt Vadge’s Double Whammy vaginal pessary blend is one example of a product that addresses both conditions. But even with dual blends, treatment should be guided by test results to avoid overtreatment or the wrong approach.
8. Key differences between AV and BV
| Feature | Aerobic Vaginitis (AV) | Bacterial Vaginosis (BV) |
|---|---|---|
| Cause | Overgrowth of aerobic bacteria | Overgrowth of anaerobic bacteria |
| Main microbes | E. coli, Streptococcus, Staphylococcus, Enterococcus | Gardnerella, Prevotella, L. iners |
| Discharge | Yellow, sometimes green, thicker | Grey-white, thin, watery |
| Odour | Foul, unpleasant, sometimes musty or sweetish | Strong fishy smell |
| Inflammation | Yes – can be severe | No – typically only ‘silent’ inflammation |
| Symptoms | Pain, redness, swelling, burning | Usually odour, may be itchy or inflamed |
| Treatment type | Anti-inflammatory, antibacterial, probiotic | Antibacterial, biofilm disruptors, probiotic |
| Prognosis | May require longer treatment | Often resolves quickly but recurs |
9. When to seek help for aerobic vaginitis
If you’ve been diagnosed with BV or thrush but treatment hasn’t helped, or symptoms like burning, inflammation, or unusual discharge persist, it’s time to revisit your diagnosis.
Aerobic vaginitis is underdiagnosed but highly treatable. A personalised plan that includes antimicrobials, probiotics, and support for tissue healing is often the best path forward.
Your body’s microbial ecosystem is delicate, so employing targeted support when it’s out of balance is the best strategy for swift resolution.
What to do next
Aerobic vaginitis is an inflammatory condition caused by aerobic bacteria, and it differs from BV in both symptoms and treatment. Accurate diagnosis matters, as the wrong approach can prolong symptoms and impact your vaginal health.
If you’re experiencing inflammation, yellow discharge, or burning and haven’t found relief, see your doctor for an accurate diagnosis and treatment recommendations. Opt for comprehensive testing and explore your AV treatment options, with many supportive integrative treatments available.
If you need help, seek support from an experienced My Vagina naturopath – we’re experts in our field and know AV inside out.
References
Gilbert G.G. Donders, Gert Bellen, Svitrigaile Grinceviciene, Kateryna Ruban, Pedro Vieira-Baptista,
Aerobic vaginitis: no longer a stranger, Research in Microbiology, Volume 168, Issues 9–10, 2017,
Pages 845-858, ISSN 0923-2508, https://doi.org/10.1016/j.resmic.2017.04.004.