Understanding and managing dyspareunia
Dyspareunia is a condition that results in painful sex, or painful penetration, but the cause can vary quite widely between women.
Dyspareunia is simply the description of a painful symptom that has its roots in a physical or psychological cause, or both, with one of the major hurdles being figuring out what the true cause is.
Dyspareunia can be thought of like a cough – it’s a symptom of something else, but the causes of coughs are different. The nature of the cough – or your pain – is what is important in trying to identify the cause.
Finding the cause is the primary objective, so the cause can be treated, alleviating the problem. In some cases, the problem will be unidentifiable and attempts to find the cause can go on for a long time. In these cases, treatments will be management only.
Symptoms of dyspareunia
With dyspareunia, there may be a complex set of symptoms that are subjective, so you describe them. Pain is one of those things we can sometimes make worse or better just by thinking it away, and dyspareunia is unfortunately categorised like this.
With anxiety, vaginal lubrication and dilation go down, resulting in a dry, tight vagina. This makes sex painful. This is going to be one of the main go-to’s by your doctors – the classic ‘it’s all in your head’.
The expectation of pain is also cited as the cause of the pain in some cases, so if you had something painful before, you expect the pain, and viola, then it comes. This seems simplistic, but it does happen.
Diagnosis of dyspareunia
First, physical causes will be examined. This includes an examination of the pelvic floor muscles, which can contract involuntarily, called vaginismus.
A diagnosis is made based on recurrent or persistent genital pain before, during or after sex that doesn’t have an obvious cause. Obvious causes may be lack of lubrication, trying to put something too big into something too small, or otherwise a diagnosis of vaginismus.
Vaginismus and dyspareunia can occur together. The dyspareunia needs to be established as acquired or ‘just born with it’ (congenital), and generalised (complete) or dependent on the situation you find yourself in.
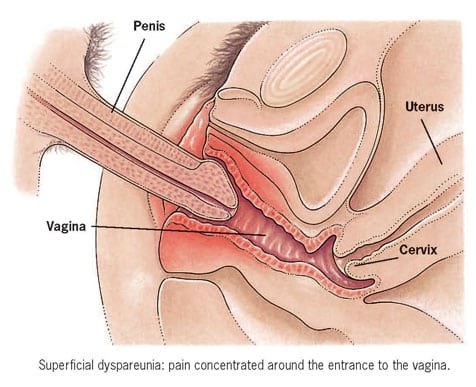
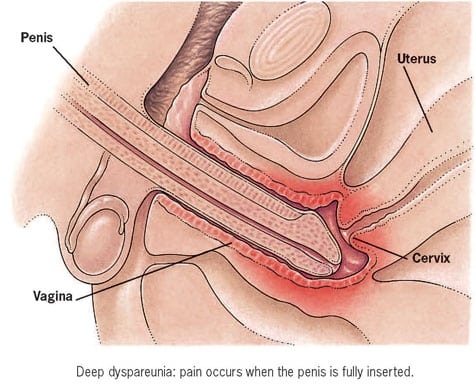
The pain will be examined: is it deep, or just on the surface, and is it just at the vaginal opening, or right inside? There has been some debate as to whether dyspareunia should be classified as a pain disorder or a sex disorder, with an acknowledgement of a pain disorder taking away the stigma from ‘women’s hysteria’ and our supposed plethora of psychological problems with sex.
As you will see, there are plenty of physical causes for it and you need to find a doctor who will take your pain seriously.
Some physical causes (congenital) of dyspareunia:
(These will occur only at first sex or attempt at penetration – they won’t appear later in life all of a sudden)
- Vaginal septum (a partition in the vaginal structure)
- A thick hymen
- Hypoplasia of the introitus (a very small, underdeveloped vaginal opening)
- Ovarian cysts, with deep pain
Some acquired physical causes of dyspareunia:
(These could occur without warning and after a happy and fulfilling sex life)
- Endometriosis, which causes masses of inflammation in the pelvis
- Infection with yeast, chlamydia, trichomoniasis, urinary tract infections or pelvic inflammatory disease
- Vulvar vestibulitis (vulva pain and inflammation)
- Tumours such as uterine fibroids
- Xerosis (dry, scaly vulva, particularly after menopause, atrophic vaginitis)
- Interstitial cystitis (IC or ‘painful bladder syndrome’)
- Uterine prolapse
- A lichenoid condition
- Female genital mutilation that has resulted in a small vaginal opening, made worse by scarring
- Episiotomy (post op stitches that are too tight)
Other conditions that can cause dyspareunia:
- Retroverted uterus
- Vaginismus
Psychological causes of dyspareunia:
- Previous trauma of any kind
- Fear and anxiety
- Unhappy relationships
- Sexual arousal disorders
- Dyspareunia is often the first sign of interstitial cystitis (IC), a painful bladder disease.
Sexual pain usually can be categorised into vulvar pain (at the entrance of the vagina or in the vaginal lips), vaginal pain, or deep pain. It is often a combination of all three.
There may be subtypes of dyspareunia, with VVS the most common type among premenopausal women, along with deep dyspareunia or pelvic pain associated with ovarian cysts, endometriosis and pelvic adhesions.
Vulvar or vaginal atrophy occurs typically in postmenopausal women. Issues might be caused by inflammation or congestion.
Treating dyspareunia
Now for the hard bit. Treating this condition can be very tricky, as you may well know. Clear discussion with a good and supportive doctor and pelvic physiotherapist is going to be the first port of call. You need to feel comfortable that they know all the details, and believe you are actually having these symptoms for real.
Keep in mind that this condition rarely sticks around forever. You are probably going to be told to learn how to touch yourself, figure out what the triggers are and avoid them if possible, have sexy baths with your partner, and caress without intercourse.
All of these are designed to loosen you up, lubricate you and get you ready to be penetrated (painlessly). You will be told to invest in some good-quality lube, applied to the penis and your vulva and vaginal opening.
These suggestions are all useful, though there are going to be some tedious conversations if you are a lifelong sex lover and know how to do all these things already.
Often this condition will appear in women who have had a healthy and happy sex life, great relationships and are mentally and emotionally healthy.
And, it can appear in women who are shy and fearful about sex, and the physical and psychological reasons can get mixed up.
You need to be clear what your thoughts are on this in conversations with your doctors, because it matters. If you think it’s physical, make sure your doctor knows why you think this. If you believe it could be psychological, seek the appropriate therapies.
If it could be a bit of both (feeding into each other), work on both elements. Don’t let your doctor tell you it’s all in your head. That’s a cop out and ignores your pain, which swift addressing.
Conditions that need to be eliminated
If you have an infection, clear that up before you start any hanky panky, because you can spread infections between you and your partner, making them harder to get rid of with standard treatment, causing your pain to go on longer.
If the pain is in deep penetration, a change of position may be suggested. If you have vaginal atrophy, oestrogen cream can be applied.
In a nutshell…
You will likely be referred to a specialist and a pelvic physiotherapist. Your treatment progress may be up to you to figure out, so keep visiting specialists until someone can help you: there has to be a reason why this is happening.
There are a lot of non-conventional practitioners – highly trained and experts in their fields – who would be happy to help you. Try pelvic physiotherapists, acupuncture, reflexology, herbal medicine, traditional Chinese medicine (TCM), osteopathy, or EFT/NLP.
Find someone you trust, and then let them take you on a ride to find out what the true cause of your pain is.