Uterine fibroids are growths (non-cancerous tumours) on the smooth muscle of the cervix or lower uterus, with the majority being small and producing no symptoms.
Sometimes the fibroids protrude through the cervical opening (the cervical os or hole) and can become ulcerous, infected, or both. Cervical or uterine fibroids vary in size, shape and number, and usually grow quite slowly and don’t cause any symptoms.
Uterine fibroids may grow in clusters, or in one nodule, ranging in size from 1mm to bigger than a watermelon. It is unclear why cervical fibroids develop, but fertile-age oestrogen levels seem to be the key indicator; prepubertal girls don’t get cervical or uterine fibroids, nor do menopausal women.
The fibrous growth is called a myoma, and when symptoms are present they can range from a feeling of pressure – urinary urgency, problems and pain urinating, sensations on the urethra, painful penetration or sex, and blockage of the cervix altogether. Painful, heavy periods may result.1,2
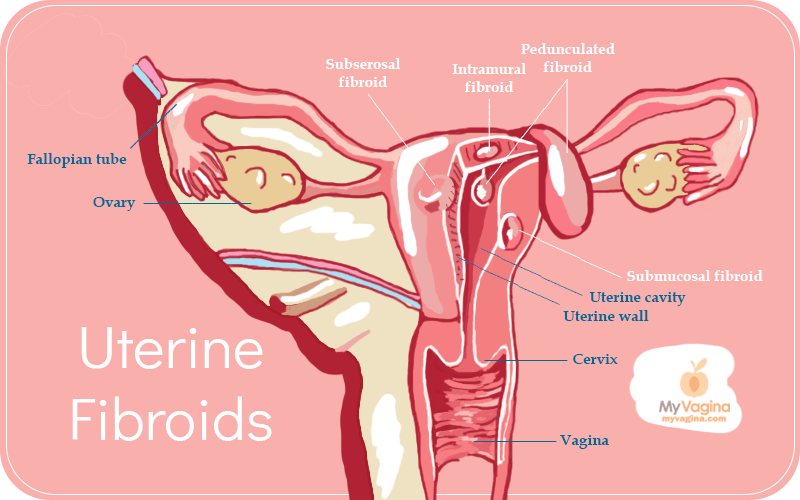
Types of uterine fibroids
- Subserosal uterine fibroids – growing in the outer portion of the uterus, growing outwards.
- Intramural uterine fibroids – these are the most common, and grow on the uterus wall, then expand, causing the uterus to feel big and bulky.
- Submucosal uterine fibroids – these grow under the uterine cavity, and can cause miscarriages and heavy periods.
- Pedunculated uterine fibroids – these fibroids grow on small stalks that join to the inside or outside of the uterus.
Uterine fibroids are usually found during an examination by a doctor, often while checking something else, but further testing may be required such as an ultrasound, to establish size and location, and monitor the growth of the fibroids. A cervical myoma that has protruded through the cervical opening (os) may look very much like a cervical polyp, and may be removed as such.
Symptoms of uterine fibroids
- Heavy periods that last a long time
- Pain or pressure in the pelvis, heaviness
- Apparent weight gain, particularly around the abdomen – may appear bulbous or bigger than seems right
- Unusual pressure or pain on the bladder, bowel or urethra, causing urinary incontinence and urgency
- Pain down the back of the legs
- Painful sex
- Smelly and/or bloody discharge
Factors that affect fibroid growth and incidence3
- Oestrogen – the more oestrogen, the greater the risk of fibroids
- Pregnancy – pregnancy seems to reduce the risk of fibroids appearing, with the more pregnancies resulting in lowered risk
- Coffee – seems may increase likelihood of developing fibroids
- Alcohol – may increase incidence of fibroids, particularly beer drinkers
- High blood pressure – may be associated with fibroid development
- Talcum powder on perineum – may increase incidence of fibroids for unknown reasons
- Obesity – associated with increased risk of fibroids (linked with higher oestrogen levels)
- Oral contraceptive use – some studies show increased risk of fibroids, others show reduced – inconclusive
- Smoking – associated with lowered incidence of fibroids
Diagnosis of uterine and cervical fibroids
Diagnosing fibroids may be achieved using your medical history and medical scans.4 Ruling out other conditions is important, and will be part of the testing.
Treatment and management of cervical and uterine fibroids
If a uterine or cervical fibroid is not growing quickly and is not producing symptoms, it is likely to just be monitored, which is the most common outcome of fibroid diagnosis.
If a fibroid is growing, quite big, or causing symptoms, you will be referred to a gynaecologist for treatment. This happens in a quarter of cases. It is important to note that fibroids are non-cancerous growths, and that ‘tumour’ does not mean cancer, but a growth.
Currently, uterine fibroids are the most common cause of hysterectomy (removal of the uterus) in women, but uterine fibroids are being increasingly managed in other ways, since just cutting the growth out does not address the underlying causes, and it leaves women without a pelvic structure.5
Uterine fibroids, due to their oestrogen-driven nature, can be managed using diet, lifestyle and oestrogen excess management strategies. 6,7
Hysterectomy is a big move, with non-surgical treatments now preferred where possible.8
MR-guided Focused Ultrasound
Treatments now include MR-guided Focused Ultrasound treatment, which leaves the uterus completely intact, but using heat, kills the fibroid cells, effectively dissolving fibroids without affecting other tissues. This is done using an MRI machine so accuracy is excellent.9
Surgical removal of fibroids
Surgery may be a hysterectomy, myomectomy, or a uterine artery embolisation. The uterine artery embolisation is a procedure performed laparoscopically whereby the blood supply to the fibroid is cut off. The fibroid will shrivel up and disappear.10–12
Drugs to reduce the size of fibroids before surgery
Drugs used to shrink fibroids have one main purpose: to reduce overall levels of oestrogen. The drugs modify hormone levels to reduce oestrogens, which may include increasing androgens, suppressing oestrogens, and inducing medical menopause.
How natural medicine can help manage fibroids
There are a few key approaches to managing fibroids and their symptoms. A natural therapist may aim to reduce heavy periods, regulate relative oestrogen excess, and either maintain or reduce the fibroid’s size.
Managing heavy bleeding
Reducing heavy bleeding may be the only outcome necessary, depending on whether childbearing years are past or not. If a fibroid will be an impedance to a successful pregnancy, other approaches may be taken.13
Herbal medicine can be very effective at reducing this excessive bleeding, using anti-haemorrhagic herbs with uterine tonics. Supplementation with iron may be appropriate for chronic heavy bleeding, which may also reduce bleeding.
Augmenting the impact of oestrogen
Understanding the impact of oestrogens is important when treating fibroids, since removal or treatment of a fibroid doesn’t mean a recurrence is impossible.
Phyto-oestrogens may be appropriate, to reduce the veracity of human-strength oestrogen in oestrogen receptors. Phyto-oestrogens are 300 times weaker than human oestrogen, so filling receptors with weak oestrogen has a net reduction in oestrogenic effect.
Clinical trials of herbal medicine in fibroids have demonstrated a positive impact in symptoms and fibroid size. Managing relative oestrogen excess is also important, and may include diet modifications, herbal medicine, and modification of lifestyle factors like exercise and smoking. Oestrogen clearance matters.
References
- 1.Mao X, Chen H, Peng X, Zhao X, Yu Z, Xu D. Dysbiosis of vaginal and cervical microbiome is associated with uterine fibroids. Front Cell Infect Microbiol. Published online September 6, 2023. doi:10.3389/fcimb.2023.1196823
- 2.Stewart E, Cookson C, Gandolfo R, Schulze‐Rath R. Epidemiology of uterine fibroids: a systematic review. BJOG. Published online May 13, 2017:1501-1512. doi:10.1111/1471-0528.14640
- 3.Donnez J, Dolmans MM. Uterine fibroid management: from the present to the future. Hum Reprod Update. Published online July 27, 2016:665-686. doi:10.1093/humupd/dmw023
- 4.Lumsden MA, Hamoodi I, Gupta J, Hickey M. Fibroids: diagnosis and management. BMJ. Published online October 13, 2015:h4887. doi:10.1136/bmj.h4887
- 5.Stewart EA, Laughlin-Tommaso SK, Catherino WH, Lalitkumar S, Gupta D, Vollenhoven B. Uterine fibroids. Nat Rev Dis Primers. Published online June 23, 2016. doi:10.1038/nrdp.2016.43
- 6.Ahmad A, Kumar M, Bhoi NR, et al. Diagnosis and management of uterine fibroids: current trends and future strategies. Journal of Basic and Clinical Physiology and Pharmacology. Published online March 30, 2023:291-310. doi:10.1515/jbcpp-2022-0219
- 7.Reis FM, Bloise E, Ortiga-Carvalho TM. Hormones and pathogenesis of uterine fibroids. Best Practice & Research Clinical Obstetrics & Gynaecology. Published online July 2016:13-24. doi:10.1016/j.bpobgyn.2015.11.015
- 8.Khan A, Shehmar M, Gupta J. Uterine fibroids: current perspectives. IJWH. Published online January 2014:95. doi:10.2147/ijwh.s51083
- 9.Dobrotwir A, Pun E. Clinical 24 month experience of the first MRgFUS Unit for treatment of uterine fibroids in Australia. J Med Imag Rad Onc. Published online April 24, 2012:409-416. doi:10.1111/j.1754-9485.2012.02376.x
- 10.Lethaby A, Vollenhoven B. Fibroids (uterine myomatosis, leiomyomas). BMJ Clin Evid. 2015;2015. https://www.ncbi.nlm.nih.gov/pubmed/26032466
- 11.Clements W, Ang WC, Law M, Goh GS. Treatment of symptomatic fibroid disease using uterine fibroid embolisation: An Australian perspective. Aust NZ J Obst Gynaeco. Published online January 20, 2020:324-329. doi:10.1111/ajo.13120
- 12.Peker N, Gündoğan S, Şendağ F. Laparoscopic Management of Huge Cervical Myoma. Journal of Minimally Invasive Gynecology. Published online March 2017:345-346. doi:10.1016/j.jmig.2016.09.002
- 13.Freytag D, Günther V, Maass N, Alkatout I. Uterine Fibroids and Infertility. Diagnostics. Published online August 12, 2021:1455. doi:10.3390/diagnostics11081455
The most comprehensive vaginal microbiome test you can take at home, brought to you by world-leading vaginal microbiome scientists at Juno Bio.
Unique, comprehensive BV, AV and 'mystery bad vag' treatment guide, one-of-a-kind system, with effective, innovative treatments.
Promote and support a protective vaginal microbiome with tailored probiotic species.