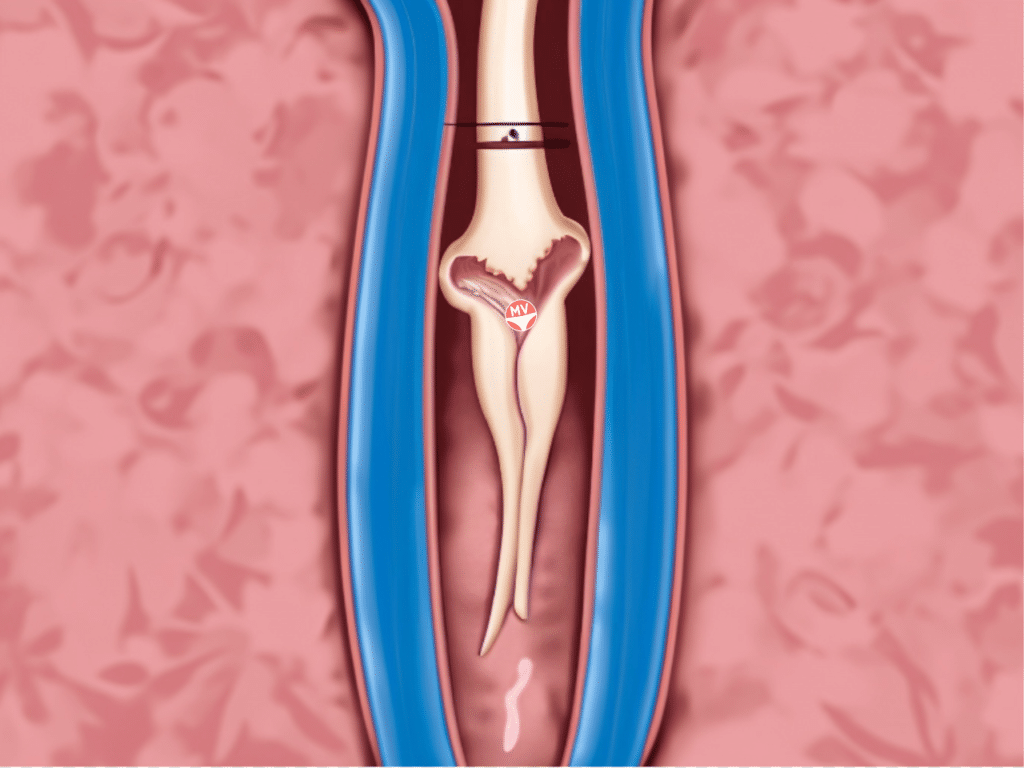
A vaginal septum is a piece of flesh inside the vaginal canal that is attached either lengthways (longitudinal) or sideways/horizontal (transverse).
These vaginal septa can go unnoticed, or can cause vaginal blockages, painful sex, impossible tampon use, and difficulties during labour.
Septum abnormalities are developed in the womb and therefore are known as congenital (or anatomical) abnormalities.
A septum is a separator of some kind, as you would see between your nostrils.
Transverse (horizontal) vaginal septum
A transverse vaginal septum occurs when a defect in fusion occurs when the vagina is being created during foetal development. The Mullerian ducts incorrectly fuse to the urogenital sinus.
A transverse vaginal septum is estimated to occur to one anatomically female person in 3,000-80,000, and is considered the rarest of urogenital tract congenital abnormalities.
Numbers are vague because if the septum doesn’t trap menstrual blood behind it in a complete obstruction, it can go completely unnoticed.
The septum is usually less than one centimetre thick. A vaginal septum is often located in the top section of the vagina, but can be found anywhere in the vagina. These vaginal septa are not generally associated with other reproductive abnormalities.
Symptoms of a transverse vaginal septum
The most noticeable problems occur around puberty and menstruation when menstrual blood accumulates behind the blockage (cryptomenorrhoea), causing cyclic abdominal pain, problems urinating and back pain.
As a newborn, unusual abdominal swelling can occur as vaginal discharge caused by the mother’s pregnancy hormones cannot escape.
Treatments for a transverse vaginal septum
Treatment for a transverse vaginal septum is typically surgery, where the excess tissue can easily be removed. The surgery is usually uneventful, quick, and complications are very, very rare.
Longitudinal (lengthways) vaginal septum – the ‘double vagina’
A longitudinal septum is also termed the ‘double vagina’, where the Mullerian ducts fuse incompletely. This makes the vagina split into two, and is often accompanied by a double cervix, and a uterine septum or double uterus (uterus didelphys).
Many of those with longitudinal vaginal septa and double organs may go their whole lives without being aware of it. Painful sex (dyspareunia) may occur as a result, in which case surgery on the septum can be performed and the problem is usually solved.
Symptoms of a longitudinal vaginal septum
A longitudinal vaginal septum may result in pain during sex or menstruation, and cause uterine bleeding. It is not dangerous to your health, and can go unnoticed for a lifetime.
Diagnosis of a longitudinal vaginal septum
MRIs are very useful for diagnosis, and are considered to be the gold standard in diagnosing the nature of a vaginal septum.
Fertility outcomes of a longitudinal vaginal septum
There is a higher risk of blood going ‘backwards’ (retrograde menstruation) due to the blood being unable to escape out of the body via the vagina.
Retrograde menstruation can result in endometriosis, whereby blood from the uterus escapes into the body cavity via the fallopian tubes and attaches to the walls of internal organs.
Those with vaginal septa can have successful pregnancies, however they tend to have slightly worse pregnancy outcomes. Conception can be difficult, and miscarriages are more common with transverse and longitudinal vaginal septa.
Those with lower transverse vaginal septa have better conception rates than those with upper or middle transverse septa.
Other problems with carrying a baby to term include early pregnancy loss, premature births, abnormal foetuses and preterm labour. Obstruction can also occur during birth, particularly if the septum has not been discovered until late in the process.
Live birth rates for longitudinal septa sit at 82 per cent, and 94 per cent for those with a transverse septum.
Surgical treatments and outcomes for vaginal septa
The septa removal surgery is reasonably straightforward as in, the septum is removed and the bases of the septum are joined together.
Your surgeon should be experienced in this surgery. The Atlas of Pelvic Surgery has an excellent set of diagrams that accurately depicts the surgery.
In terms of outcomes, the surgery will keep you in hospital for one or two days (though some are out the same day), and the tissue is healed up in weeks. Sex can resume after about four weeks.
Any surgery comes with risks, and your surgeon will explain these to you. The risks of this surgery are poor healing and scar tissue, nerve damage, and infection.
Because the surgery isn’t too invasive, risks can be minimised, and the benefits will be great – having pleasurable (pain-free) sex and if it is on the menu, conceive and deliver a baby without extra risks.
The most comprehensive vaginal microbiome test you can take at home, brought to you by world-leading vaginal microbiome scientists at Juno Bio.
Unique, comprehensive BV, AV and 'mystery bad vag' treatment guide, one-of-a-kind system, with effective, innovative treatments.
Promote and support a protective vaginal microbiome with tailored probiotic species.