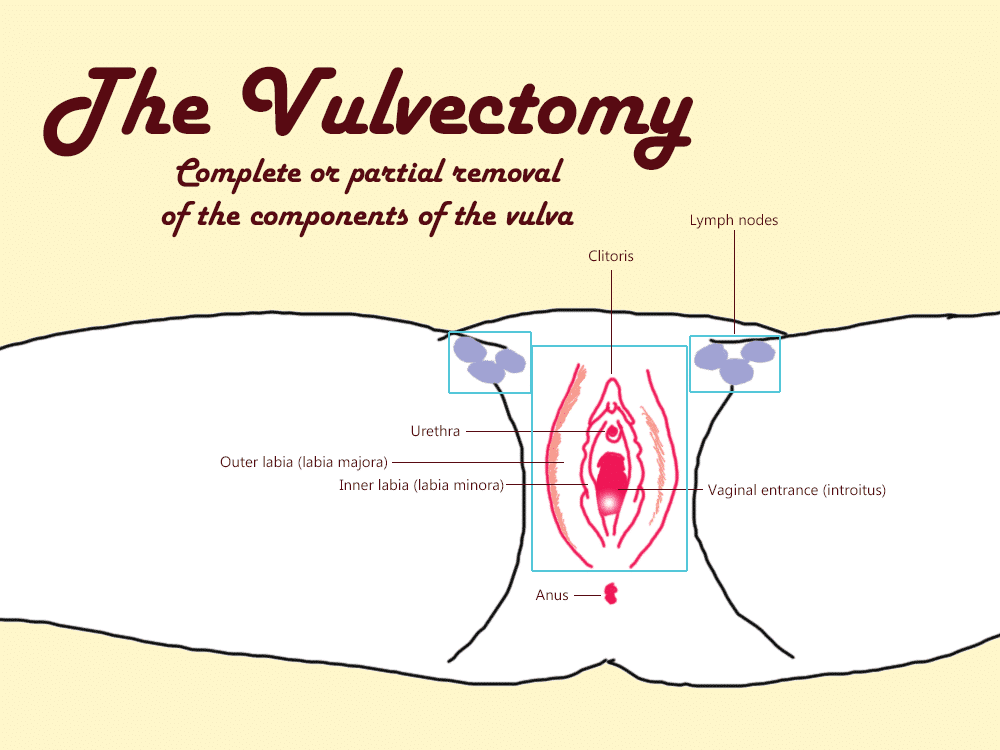
When serious disease is found on the vulva (the external area of the vagina that includes the labia and clitoris) one treatment strategy is surgery, more specifically the vulvectomy.
Vulvectomy comes from the root word ‘vulva’ and the suffix ‘-ectomy’ (meaning ‘removal’).
In essence, a vulvectomy means surgical removal of the vulva, which can be complete or partial.
Surgical techniques are improving all the time, so the outcomes of vulvar surgery are improving. Technique fine-tuning means improvements in the way your vulva looks and functions after a vulvectomy and reconstructive surgery1.
Types of vulvectomy2–6
Partial vulvectomy is the removal of only the affected part of the vulva, plus a margin of tissue surrounding the affected/diseased area.
Modified radical vulvectomy is the removal of the affected part of the vulva, a margin of tissue surrounding the affected/diseased area, plus groin lymph nodes.
Radical vulvectomy is the removal of the entire vulvar area, which includes the inner and outer lips (labia), the clitoris, lymph nodes and a margin of tissue. Radical vulvectomies are rarely performed.
Sensation after a vulvectomy
There may be some numbness in the groin area but usually the sense of feeling returns after a few weeks or months.
You may feel pain or discomfort when wearing tight pants and your genital area might look quite different than you are used to. The new look may be come as a shock.
Fertility after a vulvectomy
You should be able to get pregnant normally, but discuss this with your doctor since other treatments you are undertaking will need to be taken into consideration relating to your fertility.
Pregnancy and birth after a vulvectomy
You may be advised against a vaginal birth. You have the option to have reconstructive surgery especially if you had undergone radical vulvectomy.
Those whose groin lymph nodes had been removed might experience what is called lymphoedema, a swelling of the groin area or the legs. It’s possible in some cases that chronic pain and discomfort results from genital surgery – this is a risk.
Chronic nerve pain is a terrible suffering, and so it’s important that you have the best vulvar surgeon to help minimise the risks of nerve damage.
Make sure your surgeon has done the operation many times previously with excellent outcomes. If you have any doubts at all, and if you are able to, find another surgeon.
What you will look like after surgery
Initially, your groin area will be very swollen and bruised, but this heals up. What your vaginal area will look like will depend on how comprehensive the surgery was.
It may be shocking to look at your vaginal area without your labia, so getting used to this and learning to accept your new body is important, but will take time. Don’t expect to love it straight away, or ever necessarily. Work on, at some point, learning to accept it.
Vulvectomy and sex7
You might have a problem reaching orgasm after having a vulvectomy, depending on how much of the vulva has been removed.
The clitoris and outer lips are important components in sexual pleasure and arousal. When these are removed, the sensation is lessened in those areas. In some cases the ability to feel pleasure may be greatly diminished or absent.
There may be a few tricks to learn after a vulvectomy that aren’t what you are used to in sexual arousal and pleasure. It can take time to figure out what your body will do, so working patiently with your yourself or your partner is really important.
It may take two years or so before the area is fully healed and sex can be attempted. Slow and steady wins the race – it may take a lot longer to achieve orgasm, but it’s usually entirely possible.
One of the major hurdles for pleasurable sex is self-esteem and your feelings about the way your body looks. This is inevitable, and you will need to figure this out as you go.
Acceptance is the only way to deal with it, so focus on first grieving, and then when you’re ready, with your partner, talk about how you can move forward with your sex life and see what’s lays ahead.
Get professional help where possible, as you find your own way through the hot mess. Every couple will approach this differently, but a successful, happy, orgasmic sex life is usually possible after a vulvectomy.
Connecting with others who have been through a vulvectomy may be extremely helpful – you are not alone.
The vulvar issues that result in a vulvectomy can vary, but vulvar cancer is the most common.
Your emotional response to a vulvectomy
A vulvectomy can be really devastating, and it’s not something to be taken lightly or to think you’ll heal up from and just ‘get over’. But, some of you may be really happy to be relieved of your symptoms.
Find a support group of others who you can whinge to and celebrate your wins, to help support through your immensely difficult journey. Vulvectomy is hard, disease is hard, surgery is hard, even when it goes well, let alone when complications occur. This is a hard road for you all.
You will need some time to grieve for your old body and accept the new one, and grief counselling may be appropriate. No matter what, the feelings you are likely to experience will be grief, shock, anger, and fear, along with a loss of confidence. You may also feel deeply relieved to be disease-free.
Remember that others have gone through this and come out the other side. There is life after a vulvectomy!
References1–7
- 1.Martin A, Stewart JR, Girithara Gopalan H, Gaskins J, Fregosi N, Medlin EE. Complications of vulvar reconstruction following vulvectomy: A study of a nationwide cohort. Gynecologic Oncology. Published online June 2018:214. doi:10.1016/j.ygyno.2018.04.487
- 2.Hoffman MS, Roberts WS, Finan MA, et al. A comparative study of radical vulvectomy and modified radical vulvectomy for the treatment of invasive squamous cell carcinoma of the vulva. Gynecologic Oncology. Published online May 1992:192-197. doi:10.1016/0090-8258(92)90284-p
- 3.Kumar N, Ray MD, Sharma DN, et al. Vulvar cancer: surgical management and survival trends in a low resource setting. J Egypt Natl Canc Inst. Published online January 14, 2020. doi:10.1186/s43046-019-0015-y
- 4.Martin AL, Stewart JR, Girithara-Gopalan H, Gaskins JT, McConnell NJ, Medlin EE. Trends and Complications of Vulvar Reconstruction After Vulvectomy: A Study of a Nationwide Cohort. Int J Gynecol Cancer. Published online October 2018:1606-1615. doi:10.1097/igc.0000000000001332
- 5.He L, Chen G, Li X, et al. Safety and feasibility of single-incision radical vulvectomy: a novel approach for the treatment of vulvar cancer. Ann Transl Med. Published online February 2021:320-320. doi:10.21037/atm-20-6077
- 6.Grattarola R. Long-term Results of Vulvectomy with or without Groin Resection, in the Vulvar Carcinoma. Tumori. Published online January 1964:31-38. doi:10.1177/030089166405000104
- 7.Schultz WCMW, Wijma K, Wiel HBMV de, Bouma J, Janssens J. Sexual Rehabilitation of Radical Vulvectomy Patients: A Pilot Study. Journal of Psychosomatic Obstetrics & Gynecology. Published online January 1986:119-126. doi:10.3109/01674828609016749
The most comprehensive vaginal microbiome test you can take at home, brought to you by world-leading vaginal microbiome scientists at Juno Bio.
Unique, comprehensive BV, AV and 'mystery bad vag' treatment guide, one-of-a-kind system, with effective, innovative treatments.
Promote and support a protective vaginal microbiome with tailored probiotic species.