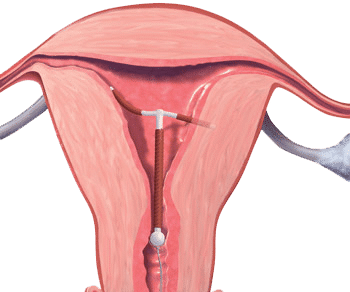
You do not have to have your IUD removed for bacterial vaginosis (BV) treatment to be successful, but if treatment is failing repeatedly, it’s worth considering.
The expense and pain involved with intrauterine device (IUD) insertion and removal is not insignificant. Many have successfully treated BV with an IUD present, but if you’re getting very heavy, long periods, the pH can be disrupted, and the source of iron in blood can provide disruptive flora with needed substrates.
Additionally, bacterial biofilm can more easily develop on the surface of the IUD and string. Biofilm-creating bacteria love a nice, smooth surface to build upon (teeth, medical implants, etc.).
We know that copper IUDs tend towards higher rates of BV and vaginal microbiome disruptions, but the Mirena and other hormonal IUDs don’t have the same risk profile.
Ultimately the choice is yours. If you have other symptoms from your IUD, such as bowel habit changes, very heavy, painful periods, back pain or mood changes, it’s worth reconsidering the IUD as your choice of birth control for now.
References1–3
- 1.Daniel AL, Auerbach S, Nazarenko D, Agbemenu K, Lorenz R. An Integrative Review of the Relationship Between Intrauterine Devices and Bacterial Vaginosis. Nursing for Women’s Health. Published online April 2023:141-151. doi:10.1016/j.nwh.2023.01.007
- 2.Brown BP, Feng C, Tanko RF, et al. Copper intrauterine device increases vaginal concentrations of inflammatory anaerobes and depletes lactobacilli compared to hormonal options in a randomized trial. Nat Commun. Published online January 30, 2023. doi:10.1038/s41467-023-36002-4
- 3.Erol O, Simavlı S, Derbent AU, Ayrım A, Kafalı H. The impact of copper-containing and levonorgestrel-releasing intrauterine contraceptives on cervicovaginal cytology and microbiological flora: A prospective study. The European Journal of Contraception & Reproductive Health Care. Published online April 17, 2014:187-193. doi:10.3109/13625187.2014.900532