A major cause of recurrent urinary tract infections (UTIs) is the build-up of oxalates in the urinary tract, particularly the ureters.
Oxalates are found in most plant foods and are produced during normal metabolism in the body. Problems can arise when the amount of oxalate consumed is high (juicing, very plant-heavy diets) or when the body cannot excrete oxalates fast enough, or a combination of both.
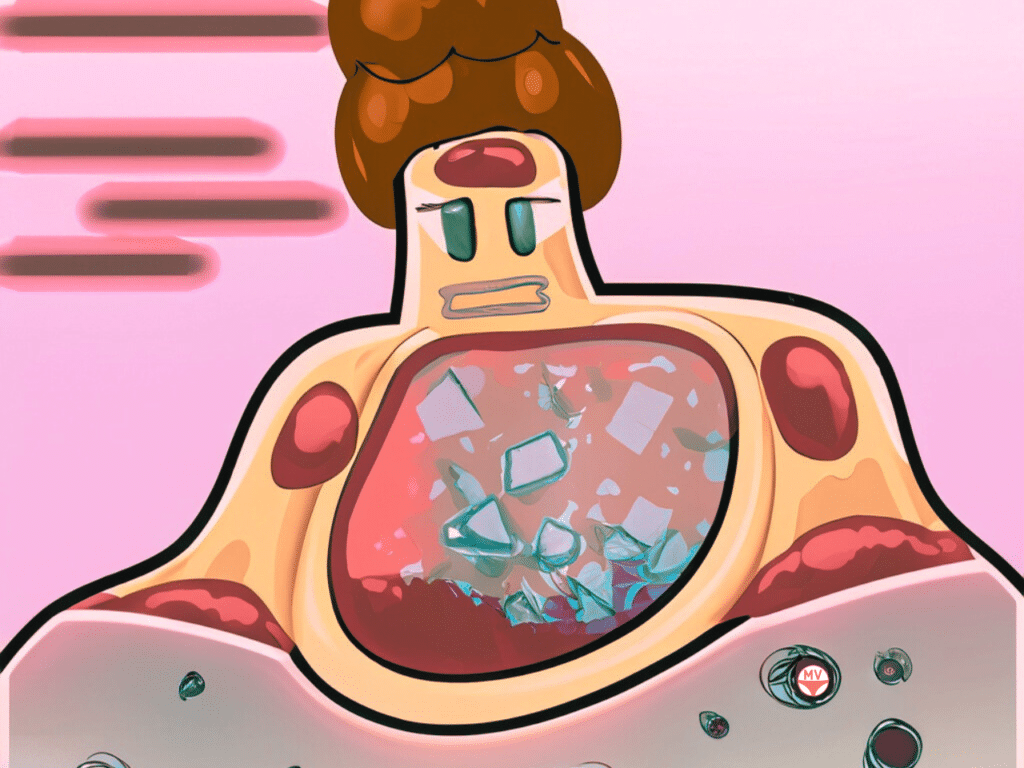
Oxalates are sharp crystals that embed themselves in tissue if not excreted properly, causing pain and other symptoms that vary in location and intensity. Major signs of oxalate overload are vulvodynia and UTIs.
Causes of oxalate buildup
- Overconsumption of high-oxalate foods like spinach, chard, beetroot, buckwheat and nuts and seeds.
- Over supplementation with vitamin C – over 500mg per day increases oxalates.
- Low vitamin B6 – B6 degrades oxalates (B6 can be low for many reasons, including ongoing infections, inflammation, and lysine deficiency)
- Poor gut health and a poor gut microbiome
- Overgrowth of Candida in the gut – Candida produces oxalates and clogs detoxification pathways
- Glyphosate (RoundUp) used as a herbicide/pesticide increases oxalates in the body by binding to many nutrients required for detoxification
Treating oxalate overload
It’s first important to establish if oxalates are an issue for you. Chronic UTIs are a key sign of an oxalate issue, but anyone with fibromyalgia, joint pain, chronic fatigue, bladder symptoms, vulvodynia, digestive pain, kidney stones (also in the family), and chronic yeast problems may have oxalate problems.
The first step is to remove high oxalate foods from your diet, but this should be done in steps to avoid a big clearance of oxalates all at once. Oxalate shards can come out of the skin and be extremely painful, so take it slow over a few weeks or months to avoid what’s known as oxalate dumping.
The first steps are to remove very high oxalate foods, and each week, graduate down from very high, to high, to medium, etc., until you are on a low oxalate diet. Use the appropriate mineral supplements advised by your practitioner.
B6 is used to remove oxalates, but usually, most people are not deficient in B6. But, just increasing B6 isn’t the answer, as this can cause more problems than it solves, so addressing all elements of your individual biology is important when treating oxalate overload. It’s not as simple as taking out the oxalates; there is a lot more to it that needs to be addressed.
If you have chronic infections or inflammation, you will likely need more glutathione, our body’s master antioxidant. This will use up more B6, as glutathione requires this B vitamin.
A lysine deficiency may also contribute to B6 deficiency. If you are getting a lot of cold sore outbreaks, you may be low in lysine.
Treat the gut – the digestive system is a major influence in terms of oxalate binding and elimination. If you have a pathogen or fungal overgrowth in the gut, your ability to break down oxalates is impaired.
Ensure plenty of lactobacilli-based probiotic foods and supplements alongside a good prebiotic to feed them. Some lactobacilli species can break down oxalate in the gut, along with our special guest, Oxalobacter formigenes, which loves oxalate, hence the name. This latter species is hard to get hold of, but hopefully, that will change in the near future.
Don’t skimp on calcium in foods! Calcium binds to oxalate and makes it unable to be absorbed. Adding good doses of calcium citrate and magnesium citrate to every meal will catch the oxalate before it can be absorbed.
Testing for excess oxalates
We might use several tests to check for oxalates: a urine test, Lactate Dehydrogenase (LD) test and an organic acids test. If you’re unsure how to get those, find an experienced practitioner who can guide you.
A urine test is a relatively simple way to measure oxalate excretion via the kidneys – high levels mean a lot of oxalates. Repeat the test to check your progress.
Oxalate in urine 5-10 times the normal range shows more than dietary absorption of oxalates, which requires support from a practitioner. One issue with this test is that many people with huge oxalate problems are not excreting them, and they are building up. Thus, a test will not be helpful.
Many systemic issues can contribute to the problem outside of just dietary oxalates. That by itself doesn’t tend to be the real issue, just a cause of symptoms.
The organic acids test has three markers for oxalates that help us establish oxalate levels, amongst many other helpful markers for overall biochemical pathway issues.
Lactate dehydrogenase (LD or LDH) under 160 may indicate further testing is required.
Seek help from a qualified, experienced practitioner for help with symptoms associated with oxalate overload.