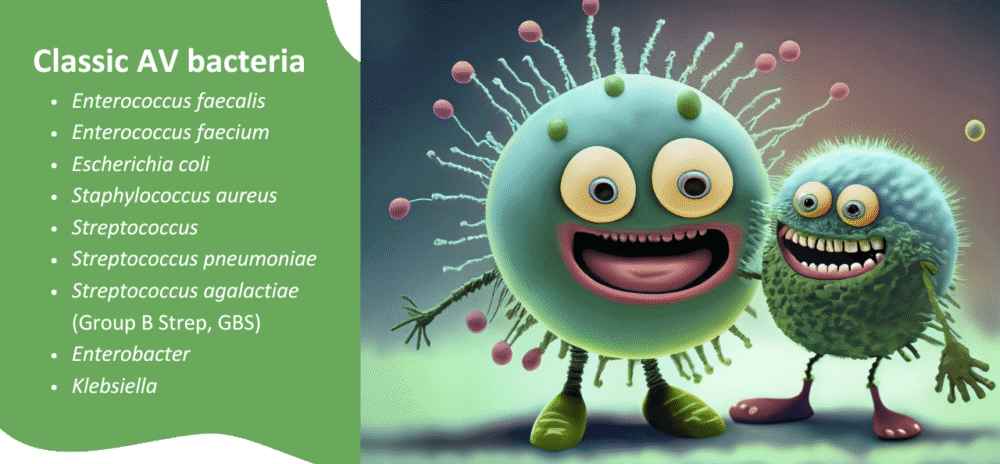
Aerobic vaginitis (AV) is a vaginal infection caused by an imbalance in the vaginal flora, where Lactobacillus species are reduced, and aerobic bacteria take hold.
AV bacteria, such as Escherichia coli, Streptococcus agalactiae, and Enterococcus faecalis1,2, can trigger significant inflammation, vaginal discomfort, and discharge. Understanding how to treat aerobic vaginitis effectively helps prevent ongoing symptoms and complications.
What is the best treatment for aerobic vaginitis?
The best aerobic vaginitis treatment3 depends on severity and test results. Most cases benefit from a combination of targeted antimicrobials (including aerobic vaginitis antibiotics if prescribed), biofilm disruption where necessary, and restoration of protective vaginal flora4.
There are several options for evidence-based medical and evidence-informed non-drug treatment of AV, with the first-line treatment typically antibiotics prescribed by a doctor.
Unfortunately, the recurrence rate of AV after antibiotic treatment is relatively high4. In My Vagina’s specialist naturopathic clinic, using a combined approach with antimicrobials and other supports tends to yield the best outcomes for AV.
Beyond antibiotics, treatments such as Fluomizin (dequalinium chloride) and probiotics may be used.
The powerful herbal formulas used in My Vagina’s clinic are targeted towards AV-causing bacteria in the vagina. While robust clinical trials in real human vaginas are still in development, we utilise scientific evidence to inform our treatment strategies.
For example, the active constituents in some herbal medicines interfere with the functions of certain bacteria, making these herbs extremely powerful treatments.
Do I have AV or something else?
A vaginal microbiome test can identify the specific bacteria involved, allowing treatment – medical or supportive non-drug treatments – to be tailored to the infection.
How long does aerobic vaginitis treatment take?
Treatment length varies depending on severity and whether symptoms have been present for weeks or months.
Most people with AV see significant improvement within 1–2 weeks when treating aerobic bacteria correctly. However, full recovery, including the rebuilding of protective vaginal flora, can take several weeks. If infections recur, longer-term support and follow-up microbiome testing are recommended.
Can aerobic vaginitis be cured permanently?
Aerobic vaginitis can be effectively treated with the right combination of antimicrobial and probiotic therapies. However, the term “cure” is misleading, as recurrence is common if the underlying imbalance is not addressed.
Supporting the vaginal microbiome with products like vaginal probiotics and monitoring pH with accurate vaginal pH strips can help prevent re-infection. Partner factors, sexual activity, and underlying health issues also need to be considered.
1. Understanding aerobic vaginitis
Aerobic vaginitis differs from bacterial vaginosis (BV). While BV is caused by anaerobic bacteria such as Gardnerella vaginalis, AV involves aerobic bacteria, which thrive in the presence of oxygen. Symptoms can include:
- Yellow or greenish discharge
- Vaginal burning, irritation, or pain
- Foul odour
- Elevated vaginal pH (>4.5) but pH may be within ‘normal’ range
- In some cases, pain during sex or bleeding due to inflammation
- Vaginal symptoms improve during menstruation (important!)
If untreated, aerobic vaginitis can increase the risk of urinary tract infections, pregnancy complications5, and discomfort during sex.
2. Diagnosing aerobic vaginitis
Diagnosis of AV6 starts with clinical assessment, pH testing, and a vaginal microbiome test. A comprehensive vaginal microbiome test can identify specific bacteria, such as E. coli or S. agalactiae. Identifying the bacteria is crucial before determining the treatment.
3. Treatment approaches
Medical options7
For moderate to severe cases, a healthcare provider may recommend aerobic vaginitis antibiotics, such as amoxicillin-clavulanate, clindamycin, or other prescription agents. These are selected based on test results and clinical guidelines. Antibiotic resistance genes may be tested for to ensure the best antibiotic choice.
Antibiotic resistance is a significant issue, with a drastic decrease in susceptibility to certain antibiotics recorded8 between 2018 and 2022 in AV patients. Lowered susceptibility was observed in the following antibiotic classes:
- Fluoroquinolones
- Penicillins
- Ampicillin – dropped from 100% in 2018 to just 43.5% in 2022
- Ciprofloxacin – dropped from 80% to 43.5% in the same period
- Trimethoprim/sulfamethoxazole saw a significant drop
The researchers found:
“E. faecalis was susceptible to vancomycin, linezolid, and teicoplanin. Ampicillin, imipenem, and ciprofloxacin had resistance rates of 22% and 5%, respectively, in the last two years.
“For S. haemolyticus strains, 0% resistance to vancomycin, linezolid, teicoplanin, and daptomycin was reported; however, in 2019, all isolates were methicillin-resistant.
“The aminoglycoside and macrolide susceptibility patterns were the opposite; gentamicin susceptibility increased in 2020 and 2021 compared to that of clindamycin and erythromycin, which showed high resistance rates from 2020 onwards (73% to 80%, respectively).”
Fluomizin, a clinically proven non-antibiotic antimicrobial, can help reduce harmful bacteria with minimal disruption of beneficial Lactobacillus species, should any remain in the vagina during an AV infection. Fluomizin is often paired with oral and vaginal probiotic treatments to support recovery.
Herbal and microbiome-focused support
Alongside medical options, several evidence-informed products can support the vaginal environment:
- Aunt Vadge’s AV Rescue – targets AV-related bacteria in the vagina
- Aunt Vadge’s Oral AV Formula – provides systemic herbal antimicrobial support targeting AV-related bacteria
- V-Spot vaginal probiotic – replenishes beneficial Lactobacillus strains
- Accurate vaginal pH strips – help monitor recovery progress if the pH was disrupted
When treating aerobic bacteria, combining antimicrobial support with microbiome restoration reduces the likelihood of infection recurrence.
Evidence-informed herbal medicine for AV
Antibiotic resistance in human bacterial and fungal pathogens is a significant public health challenge globally, making the hunt for effective alternatives urgent. These alternatives exist, and solid research exists into these botanical medicines; however, many researchers and practitioners are unsure how to use these medicinal plants safely and effectively in patients.
There can also be stigma attached to treatments perceived as ‘non-scientific’ or ‘non-medical’, despite a long history of use in traditional medicine and clear past and emerging evidence of efficacy.
An example AV herb: Sida acuta
Commonly used in My Vagina’s AV herbal formulations is a herb called Sida acuta, specifically for AV-related bacteria. Sida has been shown to have antimicrobial effects on Staphylococcus aureus and E. coli9, two common species associated with AV and UTIs.
Being researched is the therapeutic impact of sida on urinary tract infection (UTI) bacteria, for example, Staphylococcus saprophyticus, with promising results.
Researchers from a 2021 study stated10: “…S. acuta leaf extract also exhibited high antimicrobial property on all the organisms with Candida albicans showing the highest susceptibility.
“This result supports the claims of Akilandeswari et al. (2010) who also reported high zones of inhibition against the organisms tested especially against Escherichia coli, Staphylococcus aureus and Candida albicans.
“The high degree of antibacterial activity and antifungal activity thus seems to confirm the folk therapy of infections and traditional therapeutic claims of this herb.”
My Vagina’s significant clinical experience
Here at My Vagina, we only use high-quality, manufacturer-tested herbal medicines to treat infections, with a high degree of success across multiple patient groups with AV. We don’t ever use sida alone, but combine it with other powerful AV-specific herbal medicines.
These AV-effective herbs include:
- Cryptolepis (Cryptolepis sanguinolenta)
(e.g. impacts S. aureus, S. saprophyticus, E. coli, Klebsiella pneumoniae, Proteus mirabilis, Pseudomonas aeruginosa, Salmonella typhi and Salmonella typhimurium11) - Liquorice (Glycyrrhiza glabra)
(e.g. impacts K. pneumoniae, Helicobacter pylori, Streptococcus mutans, P. aeruginosa, Enterococci, Salmonella enterica, Coagulase-negative staphylococci, S. aureus12) - Green tea (Camellia sinensis)
(e.g. impacts E. coli, E. faecalis, S. aureus, C. albicans, and P. aeruginosa13)
Our practitioners may choose to use other herbs to treat AV or UTI in patients; this is not the only strategy, but rather an example to demonstrate, with evidence, the efficacy of these herbs against AV and UTI bacteria.
While none of the studies to date have been conducted in humans with AV, the robust research already undertaken, combined with our extensive clinical experience, gives us confidence in our evidence-informed strategy.
There is significant research being conducted worldwide on botanical pharmaceuticals for AV and UTI-related bacteria, so keep an eye out!
4. Rebuilding healthy vaginal flora
Treating aerobic vaginitis is not just about removing infection. It is also about restoring a Lactobacillus-dominated microbiome.
Lactobacillus crispatus, L. gasseri and L. jensenii are protective species that help maintain a healthy pH and prevent overgrowth of harmful bacteria.
Probiotic pessaries, such as the V-Spot vaginal probiotic or Life-Space Women’s Microflora Probiotic, deliver these species directly into the vagina, thereby improving resilience and helping to prevent future infections.
5. Addressing partner and lifestyle factors
Vaginal aerobic bacteria can be transmitted during sex, especially if condoms or a barrier method are not used. Partners may carry bacteria asymptomatically. Sexual activity can also alter vaginal pH, making the environment more susceptible to infection.
Using condoms or a barrier during treatment, limiting new sexual exposures, and testing and treating partners if symptoms recur can help break the cycle.
Additionally, ‘double dipping’ a penis, finger, toy or other object from the anus to the vagina without thorough cleansing first is, in My Vagina’s patient group, a huge source of AV-related bacteria transmission and infections.
Partners should be educated that this practice is a strict no-no before sex. If double-dipping happens unexpectedly during sex, stop immediately and thoroughly shower and use a vaginal probiotic to help prevent AV infection.
AV bacteria are typically found in the digestive system, allowing for easy transmission from the anus to the vagina through sex.
6. Preventing recurrence
Preventing recurrent infections may require ongoing care for susceptible people:
- Monitor pH regularly with pH testing
- Use probiotic support, such as the V-Spot vaginal probiotic, for several weeks after treatment
- Address underlying factors like low estrogen, immune health, or recent antibiotic use
- Retest the microbiome if symptoms persist
7. When to seek help
If symptoms persist despite initial treatment, or if they recur frequently, book an appointment with a My Vagina vulvovaginal specialist naturopath. They can help determine whether biofilm-forming bacteria are present and whether additional strategies are needed.
Vaginal infection treatments are not a one-size-fits-all solution, as everyone is different. If your treatment is providing the results you are after, consider another strategy, broaden your options, and seek professional support.
What to do next
If you’re struggling with symptoms of aerobic vaginitis, start with a visit to your doctor for a test, or use a comprehensive vaginal microbiome test like Juno to identify the bacteria involved. Once you have a diagnosis, you can consider your treatment strategy.
Our practitioners can help create a personalised plan to restore balance and comfort with a vaginal infection treatment made just for you. Book an appointment today to get started.
References
- 1.Jahic M. Aerobic Vaginitis Caused by Enterococcus Faecalis – Clinical Features and Treatment. Mater Sociomed. Published online 2022:291. doi:10.5455/msm.2022.34.291-295
- 2.Kaambo E, Africa C, Chambuso R, Passmore JAS. Vaginal Microbiomes Associated With Aerobic Vaginitis and Bacterial Vaginosis. Front Public Health. Published online March 26, 2018. doi:10.3389/fpubh.2018.00078
- 3.Han C, Wu W, Fan A, et al. Diagnostic and therapeutic advancements for aerobic vaginitis. Arch Gynecol Obstet. Published online November 4, 2014:251-257. doi:10.1007/s00404-014-3525-9
- 4.Mohankumar B, Shandil RK, Narayanan S, Krishnan UM. Vaginosis: Advances in new therapeutic development and microbiome restoration. Microbial Pathogenesis. Published online July 2022:105606. doi:10.1016/j.micpath.2022.105606
- 5.Han C, Li H, Han L, et al. Aerobic vaginitis in late pregnancy and outcomes of pregnancy. Eur J Clin Microbiol Infect Dis. Published online November 22, 2018:233-239. doi:10.1007/s10096-018-3416-2
- 6.Eleutério J Jr, Campaner AB, de Carvalho NS. Diagnosis and treatment of infectious vaginitis: Proposal for a new algorithm. Front Med. Published online February 9, 2023. doi:10.3389/fmed.2023.1040072
- 7.Borrego-Ruiz A, Borrego JJ. Microbial Pathogens Linked to Vaginal Microbiome Dysbiosis and Therapeutic Tools for Their Treatment. AMH. Published online May 19, 2025:19. doi:10.3390/amh70020019
- 8.Foglia F et al. Aerobic vaginitis: antibiotic resistance trend and future actions of antimicrobial diagnostic stewardship. New Microbiol. 2024;47:164-171. https://www.newmicrobiologica.org/PUB/allegati_pdf/2024/2/164.pdf
- 9.Arhin RE, Adri-Walters E, Hackman HK, Gordon PK, Appenteng MA, Gordon A. Combinative phytochemical compositions and antimicrobial activities of Xylopia aethiopica and Sida acuta extracts. German J Pharm Biomaterials. Published online May 16, 2025:21-30. doi:10.5530/gjpb.2025.1.4
- 10.Obuotor TM, Kolawole AO, Adeyanju FO, Adewumi SS. Antimicrobial activity of Sida acuta, Phyllanthus amarus and Phyllanthus muellerianus against microorganisms implicated in urinary tract infections. ijs. Published online November 22, 2021:153-168. doi:10.4314/ijs.v23i2.16
- 11.Mills-Robertson FC, Tay SC, Duker-Eshun G, Walana W, Badu K. In vitro antimicrobial activity of ethanolic fractions of Cryptolepis sanguinolenta. Ann Clin Microbiol Antimicrob. Published online June 18, 2012. doi:10.1186/1476-0711-11-16
- 12.Chen RY, Shi JJ, Liu YJ, et al. The State-of-the-Art Antibacterial Activities of Glycyrrhizin: A Comprehensive Review. Microorganisms. Published online June 6, 2024:1155. doi:10.3390/microorganisms12061155
- 13.Tariq, AL, Reyaz AL. Camellia sinensis leaves a new treatment against urinary tract infection caused by Pseudomonas fluorescens and Serratia sp. International journal of pharmaceutical sciences and research . 2013;4(3):1546-1550. https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=f17e7787b584fb358dc053fc967fc1864d2117e3







