If you’re experiencing persistent vaginal discomfort, unusual discharge, or a burning sensation, you might be dealing with chronic aerobic vaginitis (AV). This condition is relatively new in diagnostic terms and is often overlooked in favour of more well-known vaginal infections, such as bacterial vaginosis (BV) or yeast infections.
In AV, there is an imbalance in the vaginal microbiome, where protective species are significantly reduced, and disruptive aerobic bacteria, typically found in the digestive tract, thrive.
Understanding chronic aerobic vaginitis and its long-term management is crucial for maintaining vulvovaginal health and improving overall quality of life. The ultimate goal is for complete resolution of AV, but understanding and treating underlying factors is key.
What causes aerobic vaginitis?
Aerobic vaginitis is an inflammatory bacterial condition of the vagina. It’s characterised by an overgrowth of certain aerobic – meaning oxygen-loving – bacteria.
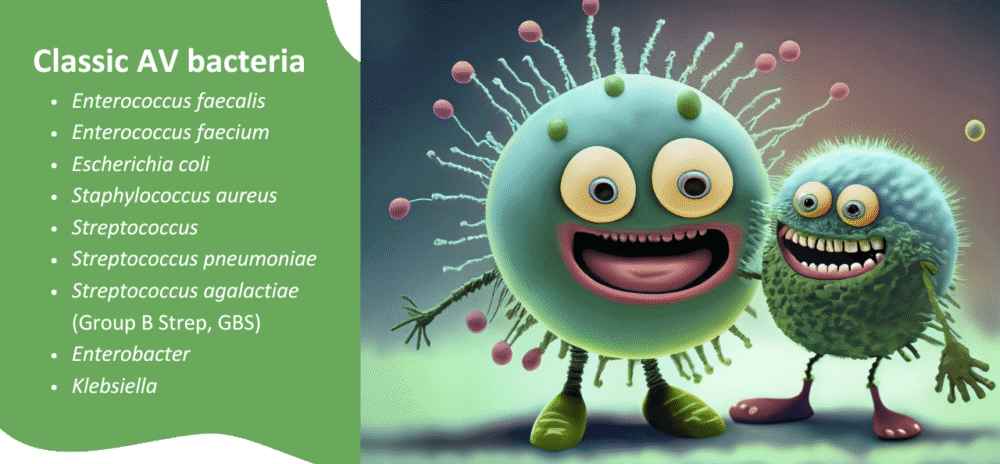
Unlike bacterial vaginosis, which often involves anaerobic bacteria, AV is characterised by organisms that thrive in the presence of oxygen. These typically include bacteria commonly found in the gut or on the skin.
Examples are Escherichia coli, Group B Streptococcus, Staphylococcus aureus, Enterococcus faecalis, and other streptococci1.
Normally, the vagina is dominated by various species of protective vaginal bacteria, primarily Lactobacillus species, especially Lactobacillus crispatus, L. gasseri, and L. jensenii.
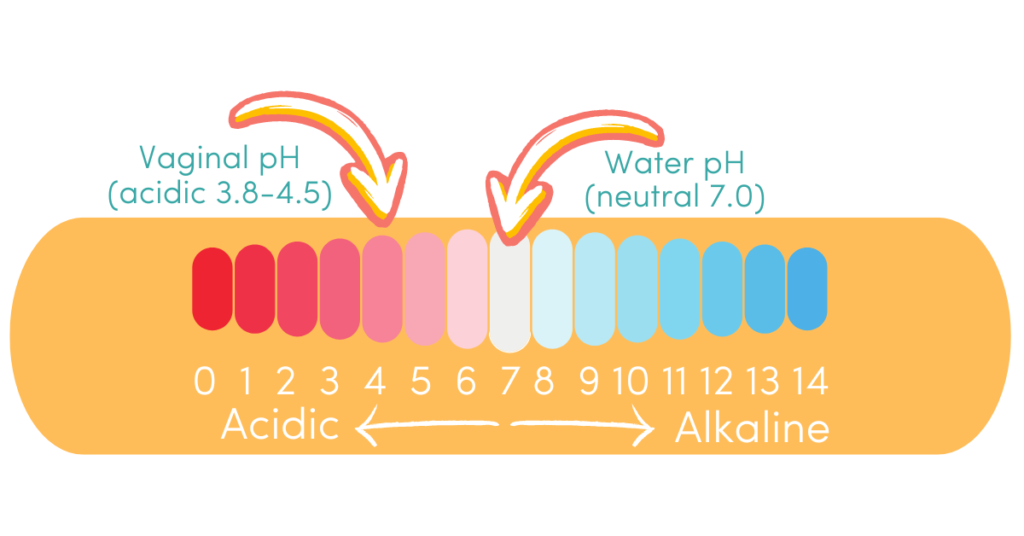
These protective bacteria produce lactic acid, which maintains an acidic vaginal pH (typically between 3.8 and 4.5). This creates an environment hostile to the growth of many disruptive bacteria.
In aerobic vaginitis, the protective dominance of Lactobacillus diminishes or disappears. This can lead to a rise in vaginal pH (often above 5.0), allowing disruptive aerobic bacteria to proliferate1. This shift triggers a local inflammatory response, leading to the characteristic symptoms.
Hot Tip: many - but not all - AV-related bacteria are also lactic acid producers. In AV, vaginal pH may not be a good indicator of infection or successful treatment.
The causes of this initial shift can be multifaceted. Factors like douching, frequent use of certain antibiotics, and even hormonal changes can disrupt the delicate vaginal ecosystem. Hormonal shifts seen in perimenopause or during breastfeeding, when oestrogen levels are lower, are examples.
The presence of persistent aerobic vaginitis can profoundly impact quality of life due to ongoing discomfort and sometimes embarrassment. Managing chronic aerobic vaginitis effectively requires a clear understanding of its distinct microbial profile.
What causes recurring aerobic vaginitis?
Recurring aerobic vaginitis can be incredibly frustrating and debilitating. Understanding the underlying reasons for its persistence is key to effective long-term management and developing strategies for aerobic vaginitis prevention.
Several factors contribute to why AV might keep coming back:
1. Incomplete treatment or misdiagnosis
One of the primary reasons for recurring symptoms is often an initial misdiagnosis or incomplete treatment. Aerobic vaginitis is frequently mistaken for bacterial vaginosis (BV) or a yeast infection due to similar symptoms like discharge, odour, and discomfort.
However, standard treatments for BV, such as metronidazole, are often ineffective against the aerobic bacteria responsible for AV1.
Treating AV effectively requires specific antimicrobial agents or approaches that target the causative aerobic organisms and address the underlying inflammation. If the initial treatment doesn’t fully eradicate the disruptive bacteria or restore the protective vaginal bacteria, the condition is likely to return. This is a common pitfall in treating chronic aerobic vaginitis.
2. Failure to restore protective vaginal bacteria
The cornerstone of a resilient vaginal microbiome is a thriving population of Lactobacillus or other protective species. In aerobic vaginitis, protective bacteria are significantly depleted and may be absent.
While eliminating the disruptive organisms is a crucial first step, it’s equally important to re-establish and support the growth of protective vaginal bacteria. Without this restoration, the vaginal environment remains vulnerable to re-colonisation by disruptive bacteria, leading to a high rate of aerobic vaginitis recurrence.
Strategies to support Lactobacillus include the use of specific probiotics and prebiotics. Protective species are essential for preventing aerobic vaginitis.
3. Presence of biofilms
Disruptive bacteria can form biofilms. These are complex communities of microorganisms encased in a protective matrix, which can adhere strongly to vaginal tissues2.
These biofilms act as a protective shield, making the bacteria highly resistant to conventional treatments. This includes antibiotics and even the body’s own immune responses.
If biofilms are present, standard treatment may only address free-floating bacteria. This leaves the protected biofilm intact to cause recurring aerobic vaginitis symptoms once treatment ceases. Specialised agents that disrupt biofilms are often necessary in such cases.
4. Immune system dysfunction
A robust local immune response within the vagina is essential for maintaining balance and fending off opportunistic infections. Chronic inflammation associated with aerobic vaginitis can sometimes signal an underlying immune system imbalance or a compromised mucosal barrier.
If the immune system isn’t functioning optimally, it can struggle to keep disruptive bacteria in check, contributing to persistent aerobic vaginitis. Factors such as chronic stress, nutrient deficiencies, and systemic inflammation can impact overall immune health, thereby indirectly affecting vaginal resilience.
5. Hormonal imbalances
Oestrogen plays a vital role in maintaining vaginal health. It promotes the growth of protective Lactobacillus and supports the integrity of the vaginal lining.
Low oestrogen levels can lead to vaginal atrophy – a thinning and drying of the vaginal tissues. This can occur during breastfeeding, perimenopause, postmenopause, or even due to certain medications.
This low estrogen environment is less conducive to the growth of protective Lactobacillus and more susceptible to the overgrowth of disruptive aerobic bacteria3. Addressing hormonal balance, where appropriate, can be a key component in preventing aerobic vaginitis.
This is particularly relevant for individuals assigned female at birth who are undergoing oestrogen blockers or high-dose testosterone as part of gender-affirming care. They may also experience symptoms of vaginal atrophy and thus be more prone to recurring vaginal infections.
6. Sexual partner impact and habits
While aerobic vaginitis is not classified as a sexually transmitted infection (STI), sexual activity can influence the vaginal microbiome. The exchange of bodily fluids during sex can introduce new bacteria or alter the vaginal pH. This potentially creates an environment where disruptive organisms can flourish.
It’s important to consider the potential role of sexual partners, especially if the partner carries relevant bacteria on their skin or urogenital area.
For individuals with penises, certain bacteria can reside on the penile skin or in the urethra. While they may be asymptomatic, they can contribute to recurring vaginal infections in their partner.
Open communication with partners and considering partner treatment strategies can be beneficial in some cases to minimise reinfection. Practising good hygiene before and after sexual activity can also be a helpful step in preventing aerobic vaginitis.
Diagnosing chronic aerobic vaginitis
Accurate diagnosis is paramount for effective long-term management of chronic aerobic vaginitis. Unlike the simple “whiff test” or pH paper used for BV, diagnosing AV often requires a more detailed assessment.
A healthcare practitioner typically performs a speculum examination to observe signs of inflammation, such as redness and swelling of the vaginal walls.
Microscopic examination of a vaginal fluid sample is important for accurate diagnosis. Under a microscope, signs of AV include a significant reduction or absence of protective Lactobacillus rods. You’ll also see the presence of various white blood cells (leukocytes), and often parabasal cells – immature epithelial cells that indicate inflammation and shedding of the vaginal lining.
The vaginal pH may be elevated, usually above 5.0.
In some cases, a comprehensive DNA-based vaginal microbiome test can provide a detailed breakdown of the bacterial species present. This helps identify the specific disruptive organisms and guide targeted treatment.
Long-term management and prevention strategies
Effective management of chronic aerobic vaginitis focuses on a multi-pronged approach: reducing inflammation, eradicating disruptive bacteria, and critically, restoring and maintaining a robust population of protective vaginal bacteria.
Aerobic vaginitis prevention involves creating an environment that naturally supports a healthy vaginal microbiome.
1. Targeted antimicrobial support
Antibiotics for AV
Given that AV involves specific aerobic bacteria, the initial approach often includes targeted antimicrobial support4. Antibiotics are the primary medical approach available, but these medicines have several key issues if initial treatment fails.
Importantly, antibiotic resistance is dramatically reducing the susceptibility of AV-related bacteria to antibiotic treatment. Data show that the susceptibility of several antibiotic classes has been reduced by over 50% from 2018 to 20225.
In addition, many antibiotic treatments fail, and AV recurs, perpetuating the antibiotic resistance issues. This treatment failure suggests that an underlying factor may not have been adequately addressed, even if the antibiotics initially work, which is where taking a more holistic, integrative approach can make all the difference.
It’s also important to understand that many antibiotics further deplete beneficial Lactobacillus species. Specific agents should be selected based on diagnostic testing results.
Herbal and non-resistance-forming antimicrobials
Topical preparations designed to address the overgrowth of aerobic organisms, such as Fluomizin (dequalinium chloride), work by targeting disruptive bacteria and dissolving biofilms, and can be highly effective in treating AV6.
Aunt Vadge’s AV Rescue is another example of a topical support option that can be considered. AV Rescue is a naturopathically developed AV-targeted preparation, featuring herbs and ingredients that interfere with specific aerobic bacterial functions while supporting vaginal health and tissue integrity.
For systemic support, Aunt Vadge’s Oral AV Formula can be helpful in addressing bacteria that may originate from other areas, such as the gut.
2. Restoring the vaginal microbiome
This is arguably the most crucial step in preventing aerobic vaginitis recurrence. Re-establishing protective vaginal bacteria helps to lower vaginal pH and create a natural defence against disruptive organisms.
Probiotics
Specific vaginal probiotics containing Lactobacillus crispatus, Lactobacillus gasseri, Lactobacillus jensenii, or Lactobacillus rhamnosus and Lactobacillus reuteri can be highly beneficial.
Products like V‑Spot vaginal probiotic suppositories deliver these beneficial bacteria directly to the vaginal environment. Oral probiotics, such as Life‑Space Women’s Microflora Probiotic, can also contribute to the overall balance, as the gut microbiome plays a role in vaginal health.
Prebiotics
Prebiotics act as food for protective bacteria. Aunt Vadge’s Lactulose Vaginal Prebiotic can selectively feed Lactobacillus species, encouraging their growth and dominance. Combining lactulose with probiotics, as found in Aunt Vadge’s Lactulose & Probiotic Kit, can provide comprehensive support.
Vaginal pH support
Maintaining an acidic vaginal pH may be important. Regular use of vaginal pH test strips can help monitor vaginal pH levels accurately. If pH remains elevated, strategies that encourage lactic acid production by protective bacteria are vital.
3. Addressing inflammation and mucosal health
Chronic aerobic vaginitis is characterised by significant inflammation. Reducing this inflammation is key to symptom relief and tissue healing.
Anti-inflammatory support
Herbal remedies and nutrients with anti-inflammatory properties can be beneficial. The AV Rescue preparation contains anti-inflammatory ingredients.
Hormonal support
If suboptimal or low estrogen is identified as a contributing factor, particularly in perimenopause or breastfeeding, topical or oral support may be considered.
Aunt Vadge’s Fennelope Intimate Restorative, which contains ingredients like phytoestrogenic fennel and sea buckthorn, can help support vaginal tissue integrity and moisture, promoting a healthier environment.
Sea buckthorn oil, applied topically or taken orally, can also be beneficial for mucosal health. Other targeted herbal supports can make a huge difference by stimulating natural hormone production or providing weaker plant estrogens. See a My Vagina practitioner for a personalised practitioner-only herbal prescription.
4. Biofilm management
If testing suggests the presence of biofilms, strategies to disrupt these protective bacterial structures are crucial for achieving and maintaining long-term vaginal health.
Products containing enzymes, such as InterFase Plus or N-acetylcysteine (NAC), can help break down biofilms, making the embedded bacteria more susceptible to other treatments. Aunt Vadge’s Biofilm Enzyme Blend and Aunt Vadge’s Nattokinase are also options for systemic biofilm support, while AV Rescue contains a targeted topical biofilm ingredient.
5. Lifestyle and hygiene considerations
Certain lifestyle practices can significantly impact aerobic vaginitis prevention:
Avoid irritants
Steer clear of harsh soaps, perfumed products, vaginal douches, and scented feminine hygiene products. These can strip away protective bacteria and irritate the delicate vaginal lining.
The inside of the vagina doesn’t need cleaning, and gentle washing of the vulva with plain water and a specific low-irritant vulva cleanser is usually sufficient.
Breathable underwear
Opt for cotton underwear, which allows for better air circulation and reduces moisture, creating a less hospitable environment for disruptive bacteria.
Sexual hygiene
Encourage partners to practise good hygiene before and after sexual activity. If you notice a pattern of recurring vaginal infections after intercourse, discuss this with your practitioner. Your partner(s) may need treatment.
Additionally, never double-dip a penis, toy or fingers from the anus to the vagina without thoroughly washing first. AV bacteria are also gut bacteria, and translocation from the rectum to the vagina is a common cause of AV we see in our clinic. Make sure partners know this rule. Be strict.
Immune support
A strong immune system can better ward off infections. Ensuring adequate nutrition, managing stress, and getting sufficient rest contribute to overall immune resilience. Eat well, sleep well and relax often – easy to say, not always easy to do! Get immune support from a naturopath or functional medicine doctor.
Addressing partner factors
For recurring aerobic vaginitis, particularly if sexual activity seems to be a trigger, consider whether a partner might be contributing to the bacterial imbalance. While My Vagina focuses primarily on vaginal health, we also offer guidance for men and people with penises.
Our Killing BV Penis Treatment Guide is designed to address potential partner involvement in vaginal microbiome imbalances, including AV. My Vagina has the world’s first and only penis treatment guide, which has been around for over a decade.
Why does aerobic vaginitis keep coming back?
The persistent nature of chronic aerobic vaginitis often stems from the interplay of the factors mentioned above. It’s rarely a simple case of a single infection that can be cleared with a quick course of medication, which puts it apart from other vaginal infections.
The complex ecology of the vaginal microbiome, individual immune responses, hormonal influences, and even the presence of resistant biofilms all contribute to the challenging cycle of recurring symptoms.
One crucial aspect is the Lactobacillus depletion. When these protective bacteria are severely diminished, the vaginal environment loses its natural protection. It then becomes highly susceptible to colonisation by disruptive bacteria.
Even if disruptive bacteria are temporarily reduced, without the re-establishment of a dominant Lactobacillus population, the vagina remains vulnerable, leading to a quick return of symptoms. This is a key reason for aerobic vaginitis recurrence.
Furthermore, the inflammatory nature of AV itself can create a vicious cycle. Inflammation can damage the vaginal epithelium, making it even harder for protective bacteria to adhere and thrive. It could also make the tissues more permeable to disruptive organisms or their toxins. This can lead to a persistent low-grade infection that flares up under various triggers.
Many individuals experience significant distress due to persistent vaginal issues, including shame and frustration. This stress can further impact the immune system, potentially exacerbating the problem.
Comprehensive care, which includes emotional support and addressing the full spectrum of contributing factors, is therefore vital for long-term resolution of recurring vaginal infections.
You are not alone! We understand AV
Chronic aerobic vaginitis is a complex and often frustrating condition. It requires a thorough, individualised approach for effective long-term management and prevention.
It goes beyond simply treating symptoms. It involves understanding the underlying imbalances in the vaginal microbiome, addressing inflammation, supporting immune function, and considering external factors like sexual health and hygiene. It could also be related to genetic variations that predispose someone to overgrowths of certain bacteria all across the body.
By implementing targeted strategies that restore the vaginal ecosystem and promote overall vulvovaginal health, individuals can break the cycle of recurring aerobic vaginitis and achieve lasting relief.
What to do next
If you suspect you have chronic aerobic vaginitis or are experiencing persistent vaginal discomfort, the first step is always accurate diagnosis. We recommend exploring a comprehensive vaginal microbiome test, especially if you’ve had inconclusive results from standard tests. This can provide invaluable insights into the specific bacteria present.
For personalised guidance on long-term management and prevention strategies, consider booking an appointment with one of our specialist naturopaths here at My Vagina. You can also complete a free support assessment to help us understand your needs – find the details in our free Killing BV Vagina Treatment Guide.
Killing BV provides comprehensive information and strategies for AV, focusing on restoring balance to the vaginal microbiome. Our clinic also offers a range of specific products to support your journey towards long-term vaginal health, including personalised practitioner prescriptions.
References
- 1.Donders, GGG, Vereecken Annie , Bosmans E, Dekeersmaecker A, Salembier G, Spitz B. Definition of a type of abnormal vaginal flora that is distinct from bacterial vaginosis: aerobic vaginitis, . BJOG: An International Journal of Obstetrics and Gynaecology. 2002;109(1):34-43. https://www.sciencedirect.com/science/article/pii/S1470032802004329
- 2.Vieira-Baptista P, Lima-Silva J, Pinto C, et al. Bacterial vaginosis, aerobic vaginitis, vaginal inflammation and major Pap smear abnormalities. Eur J Clin Microbiol Infect Dis. Published online January 25, 2016:657-664. doi:10.1007/s10096-016-2584-1
- 3.Brotman RM, Shardell MD, Gajer P, et al. Association between the vaginal microbiota, menopause status, and signs of vulvovaginal atrophy. Menopause. Published online November 2018:1321-1330. doi:10.1097/gme.0000000000001236
- 4.Tempera G, Furneri PM. Management of Aerobic Vaginitis. Gynecol Obstet Invest. Published online 2010:244-249. doi:10.1159/000314013
- 5.Foglia F et al. Aerobic vaginitis: antibiotic resistance trend and future actions of antimicrobial diagnostic stewardship. New Microbiol. 2024;47:164-171.
- 6.Tekgunduz SE, Saracoglu F. Evaluation of the effectiveness of dequalinium chloride vaginal tablets in aerobic vaginitis: A placebo-controlled study. Eastern J Med Sci. Published online October 24, 2021:50-56. doi:10.32677/ejms.v6i3.3090