Recent studies show that obesity is associated with bacterial vaginosis (BV), but the exact mechanisms are not fully understood. We take a closer look at the science to see why excess fat deposits in a body may create an environment where chronic imbalances in the vaginal microbiome can occur.
We also run you through what you can do if you find yourself in this position.
Fat is active immunological tissue
Fat is an active substance in our bodies; in fact, fat – adipose tissue – is now known to be especially active in people living with obesity.
When a large portion of your body is only one type of tissue (fat), and that tissue becomes active in some way, its impact is comparatively huge. The immune function of fat is compounded, causing a much greater effect on the rest of the body than it should.
Obesity and our response to pathogens
We know that obesity is linked with an impaired ability to defend ourselves from pathogens. We know those in our communities living with obesity are at an increased risk of being affected by outbreaks, with a good example being recent flu epidemics: people living with obesity saw an increased risk of being affected.
The response to vaccines is also impaired by obesity, limiting the usefulness of vaccination in this population.
Basically, we know that people living with obesity are more prone to infection, which means compromised immunity. Compromised immunity makes it more difficult for your immune system to not only defend itself but to recover, resulting in chronic BV. In these cases, it won’t really matter what you do; you’re pushing dung uphill.
The relationship of insulin resistance and inflammation
Obesity leads to insulin resistance, which has been postulated to be an adaptive mechanism to reduce weight gain.
If your cells won’t take up the glucose, you can’t gain weight as quickly, which is what essentially happens in insulin resistance. Your body is resistant to the effects of insulin in opening up cells to put glucose in, leaving the glucose in the bloodstream.
The damaging effect of free-floating sugar in your blood is inflammation.
The specifics of this are complex, so if you’re interested we recommend taking a deep dive into the fantastic scientific study by Grant and Dixon (2015) about fat as an immunological agent.
How to manage BV if you are living with obesity
Managing BV in obesity is going to be multifactorial. At My Vagina, we suggest you immediately stop spending money on treatments and get some solid advice on how to reduce inflammation, improve your immunity, manage insulin resistance, and, yes eventually, figure out what losing weight looks like for you to stop the merry-go-round of pathogens.
We can help you! Our online naturopaths are well-equipped to provide expert moral and physical support.
We understand that this isn’t a quick fix scenario, nor do we think we are going to cure you overnight – we build a relationship with you that we honour every step of the way with our expertise and compassionate care. We’ll stand by you as we help you chip away at the causes of your BV. Obesity is NOT too big.
Check the calendar in the Bookings section for a private, personal chat at a time that suits you.
Insulin resistance in a nutshell
Insulin resistance can be tricky to understand, but you can think of it like this…
You eat sugar >
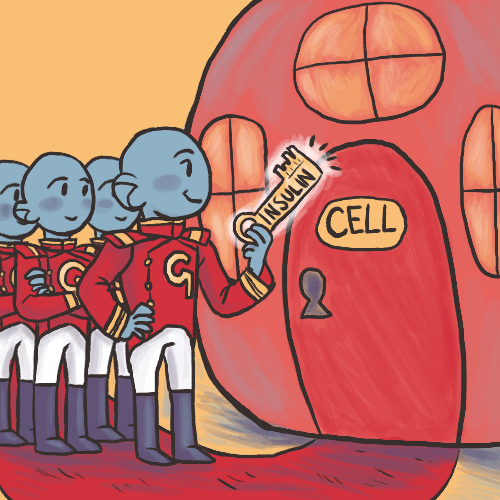
Pancreas secretes insulin to mop up the sugar out of your blood >
Insulin acts like a key to unlock cells to put sugar in >
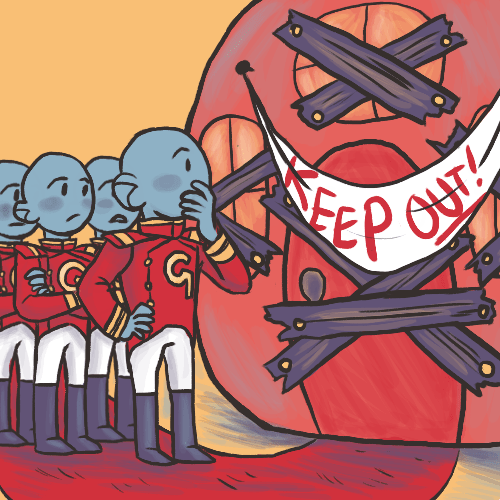
If you’re insulin resistant, the cells stop opening up as often >
Which leaves sugar in the blood for longer >
Which is dangerous to the rest of your cells because >
Sugar in the blood causes inflammation
Understanding obesity as an inflammatory condition
Obesity is characterised by excess body fat deposits, causing a body mass index (BMI) of more than 30 kg/m2. There is evidence that obesity is a low-grade inflammatory state, with fat (adipose tissue) being an active immunological organ.
Obesity has long been understood to increase our susceptibility to infections. Obesity causes adipose tissue to become inflamed, which in turn has secondary effects such as contributing to insulin resistance, diabetes and metabolic syndrome.
Immune cells such as B cells, T cells, macrophages and neutrophils have been identified in adipose tissue and obesity has been observed to influence the quantity and nature of immune cell subtypes.
Fat is a large immunologically active organ in obesity, with characteristics of both the innate and adaptive immune response.
Healthy and unhealthy obesity
There is a distinction between metabolically unhealthy and healthy obesity, with those people understood as living with healthy obesity having similar metabolic markers similar to metabolically healthy lean people. You can also have a metabolically unhealthy lean person too.
It isn’t understood what the infection implications are for people living with and without obesity who are metabolically healthy or unhealthy, with further research required. Is inflammation the key to infection, rather than obesity as a marker?
Study #1 – Association between obesity and BV – it exists
North American researchers examined the health history of almost 6,000 people, 28 per cent of whom were positive for BV. There is an association between the incidence of BV and BMI.
- Lean participants = 21 per cent had high Nugent scores (BV)
- Overweight participants = 30 per cent had high Nugent scores (BV)
- Obese participants = 35 per cent had high Nugent scores (BV)
- Intermediate flora (could go either way – BV or healthy) was found evenly distributed across all body types
In the study, obese Caucasian North Americans had significantly more BV than their leaner counterparts, while this difference was not observed in North Americans of African descent.
The vaginas in people of African descent experience a greater incidence of BV overall due to naturally low numbers of protective lactobacilli.
Study #2: Obesity and BV
Non-pregnant fertile-aged patients with a history of recurrent vulvovaginal bacterial infections and age-matched controls were included in t
Researchers determined that obesity might be an independent risk factor for recurrent/chronic vulvovaginal infections due to altered vaginal immunity.
References
Am J Obstet Gynecol. 2019 May;220(5):476.e1-476.e11. doi: 10.1016/j.ajog.2019.01.229. Epub 2019 Jan 29. Association between obesity and bacterial vaginosis as assessed by Nugent score. Brookheart RT, Lewis WG, Peipert JF, Lewis AL, Allsworth JE.
Ventolini G, Khandelwal N, Hutton K, Lugo J, Gygax SE, Schlabritz-Loutsevitch N. Obesity and recurrent vulvovaginal bacterial infections in women of reproductive age. Postgrad Med J. 2017;93(1099):297. doi:10.1136/postgradmedj-2016-134638
Physiol Res. 2015;64 Suppl 2:S105-19. Obesity and infection: reciprocal causality. Hainer V1, Zamrazilová H, Kunešová M, Bendlová B, Aldhoon-Hainerová I.
Del Cornò M., D’Archivio M., Conti L., Scazzocchio B., Varì R., Donninelli G., Varano B., Giammarioli S., De Meo S., Silecchia G., Pennestrì F., Persiani R., Masella R., et al Visceral fat adipocytes from obese and colorectal cancer subjects exhibit distinct secretory and ω6 polyunsaturated fatty acid profiles and deliver immunosuppressive signals to innate immunity cells. Oncotarget. 2016; 7: 63093-63105.
Del Cornò M, D’Archivio M, Conti L, et al. Visceral fat adipocytes from obese and colorectal cancer subjects exhibit distinct secretory and ω6 polyunsaturated fatty acid profiles and deliver immunosuppressive signals to innate immunity cells. Oncotarget. 2016;7(39):63093–63105. doi:10.18632/oncotarget.10998
Obesity (Silver Spring). 2015 Mar;23(3):512-8. doi: 10.1002/oby.21003. Epub 2015 Jan 22. Adipose tissue as an immunological organ. Grant RW1, Dixit VD.