Skene’s glands in females: location and function
Skene’s glands are small paraurethral glands located around the lower end of the urethra on the anterior vaginal wall. They are sometimes called the female prostate because they share embryological origins with the male prostate and can produce prostate-specific antigen (PSA)1.
The Skene’s glands open into or near the urethra and secrete fluid that may contribute to lubrication and, in some people, ejaculation. In most women, Skene’s glands are small, not easily visible, and do not cause symptoms.2
Skene’s gland cancer symptoms and risks
Skene’s gland cancer is extremely rare, with fewer than a few dozen cases reported worldwide3–5. Because of its rarity, it is often misdiagnosed as a urinary tract infection, a urethral diverticulum, or a vaginal wall cyst.
Typical symptoms include:
- A persistent lump or swelling near the urethra
- Pain or pressure in the anterior (front) vaginal wall
- Blood in the urine or unusual discharge
- Urinary urgency, frequency, or difficulty emptying the bladder
- Recurrent urinary tract infections that do not respond to treatment
Risk factors for developing cancer in a Skene’s gland
There are no proven risk factors for Skene’s gland cancer. Most reported cases have occurred in women over the age of 40.
Because Skene’s glands are related to the prostate1, some tumours demonstrate similar behaviour, including PSA production. This similarity explains why a few cases have responded to hormone-based therapies, though evidence is limited.
Diagnosis of Skene’s gland cancer
Assessment begins with a doctor taking a thorough medical history and doing an examination. If a lump is detected, certain tests may be recommended, including:
- Urine tests and swabs to rule out infection
- Pelvic MRI to evaluate whether the lesion is a cyst, abscess, diverticulum, or tumour
- Cystoscopy or urethroscopy to visualise the urethra internally
- Biopsy to confirm the diagnosis and determine the type of tumour
- PSA testing in some cases, since Skene’s tissue can produce PSA
Diagnosis is essential to distinguish benign cysts from malignancy and to ensure appropriate treatment.
Treatment options for Skene’s gland carcinomas
Because so few cases exist, there is no single standard treatment pathway.
Reported treatments for Skene’s gland cancers include:
- Surgical removal of the tumour
- Radiation therapy, either alone or after surgery
- Chemotherapy in selected situations
- Hormonal (androgen-deprivation) therapy in tumours that express PSA or resemble prostate adenocarcinomas
Prognosis depends on the stage at diagnosis and tumour biology. Reliable survival statistics are not available due to the very small number of documented cases. Early recognition and treatment provide the best chance of a positive outcome.
Skene’s gland cysts: causes, signs and treatments
Skene’s gland cysts are far more common than cancer. They form when the duct becomes blocked, often due to inflammation or infection.
Common symptoms of Skene’s gland cysts include:
- A smooth lump at the urethral opening that may fluctuate in size
- Pressure, discomfort, or pain with sex or sitting
- Urinary urgency, dribbling, or a stop–start stream
- A visible swelling at the anterior vaginal opening
For more, see our guide on understanding skene gland cysts.
How are Skene’s gland cysts treated?
Most Skene’s gland cysts are benign and straightforward to manage. A doctor will recommend treatment depending on size, symptoms, and whether an infection is present.
- Watchful waiting – small, painless cysts can be monitored if they are not causing problems
- Targeted antibiotics – if the cyst is infected or forms an abscess, cultures can guide antibiotic choice; antibiotics alone rarely resolve a blocked duct without drainage
- Drainage or marsupialisation – for painful, persistent, or recurrent cysts or abscesses, opening the duct to create a drainage pathway is effective
- Excision – surgical removal of the cyst or involved duct is considered if cysts recur frequently
- Imaging or biopsy – if the lump is firm, fixed, ulcerated, rapidly enlarging, or unusual, further imaging and biopsy may be recommended
- Aftercare and recurrence – sitz baths, rest, and hygiene aid recovery; report any new swelling, fever, or ongoing urinary symptoms since recurrence can occur and is treatable
Understanding Skene’s gland anatomy in women
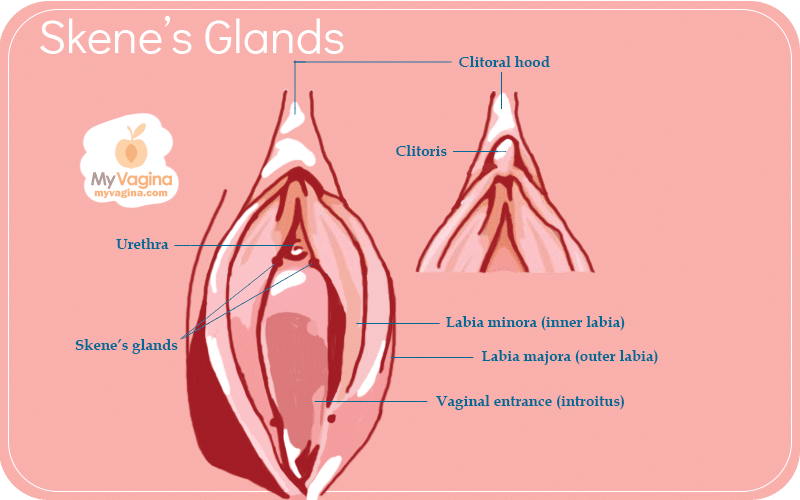
Anatomy is easier with a visual reference. Our skene’s glands anatomy diagram shows the glands around the urethra, their duct openings, and their relationship to the surrounding tissue.
Skene glands in females are positioned close to the urethral opening. This location explains why their symptoms can resemble urinary tract problems or vaginal wall issues. A cyst pressing on the urethra may cause urinary changes, while a tumour can mimic a diverticulum. Because of this overlap, imaging and biopsy are essential when a lump is not straightforward.
What to do if you see Skene’s gland cancer signs
Skene glands in females are normal structures. Problems are uncommon, and cancer is very rare. Most issues are due to benign Skene gland cysts. Still, ongoing or unusual symptoms deserve assessment.
If you have persistent symptoms, seek an evaluation by a doctor experienced in this area. Accurate diagnosis is the key to effective management and peace of mind.
Skene’s gland cancer FAQ
They are paraurethral glands located around the lower end of the urethra on the anterior vaginal wall. See our Skene’s glands anatomy diagram and Skene’s gland location in females for more detail.
A persistent lump near the urethra, pain or pressure in the vaginal wall, urinary changes such as urgency or frequency, blood in urine, or recurrent UTIs that do not improve with antibiotics.
It is extremely rare, with fewer than a few dozen cases reported worldwide. Most lumps in this area are benign, such as Skene’s gland cysts.
Evaluation may include a medical history and examination, urine tests and swabs, pelvic MRI to define the lesion, cystoscopy or urethroscopy to inspect the urethra, and a biopsy of any suspicious tissue. PSA testing may be considered because Skene’s tissue can produce PSA.
A Skene’s gland cyst is a blocked duct and is usually benign. Cancer is malignant and very rare. Imaging and biopsy are required to distinguish cysts from tumours.
Options include monitoring small cysts, antibiotics for infection, drainage or marsupialisation for persistent cysts, excision if cysts recur, and imaging or biopsy if the lump has atypical features.
Treatment may involve surgical excision, radiation therapy, chemotherapy in selected cases, and hormone therapy for tumours that behave like prostate-type cancers. The plan depends on tumour type, stage, and individual factors.
Seek medical assessment if you notice a persistent lump near the urethra, urinary changes, unexplained bleeding, pain or pressure that does not improve, or recurrent urinary infections.
References
- 1.Kaufman ME, Miller DT, Ullah A, et al. Skene’s Gland Adenocarcinoma: Borrowing From Prostate Cancer Experience for the Evaluation and Management of a Rare Malignancy. Urology. Published online May 2021:182-187. doi:10.1016/j.urology.2020.05.032
- 2.Dagur G, Warren K, Imhof R, Gonka J, Suh Y, Khan SA. Clinical implications of the forgotten Skene’s glands: A review of current literature. Polish Annals of Medicine. Published online June 2016:182-190. doi:10.1016/j.poamed.2016.02.007
- 3.Kyriazis G, Varughese A, Rodrigues G, Simms M. A Rare Case of Skene’s Gland Adenocarcinoma. Clinical Genitourinary Cancer. Published online June 2020:e300-e302. doi:10.1016/j.clgc.2019.11.022
- 4.Slopnick EA, Bagby C, Mahran A, et al. Skene’s Gland Malignancy: A Case Report and Systematic Review. Urology. Published online July 2022:36-43. doi:10.1016/j.urology.2022.02.004
- 5.Tregnago AC, Epstein JI. Skene’s Glands Adenocarcinoma. American Journal of Surgical Pathology. Published online November 2018:1513-1521. doi:10.1097/pas.0000000000001108