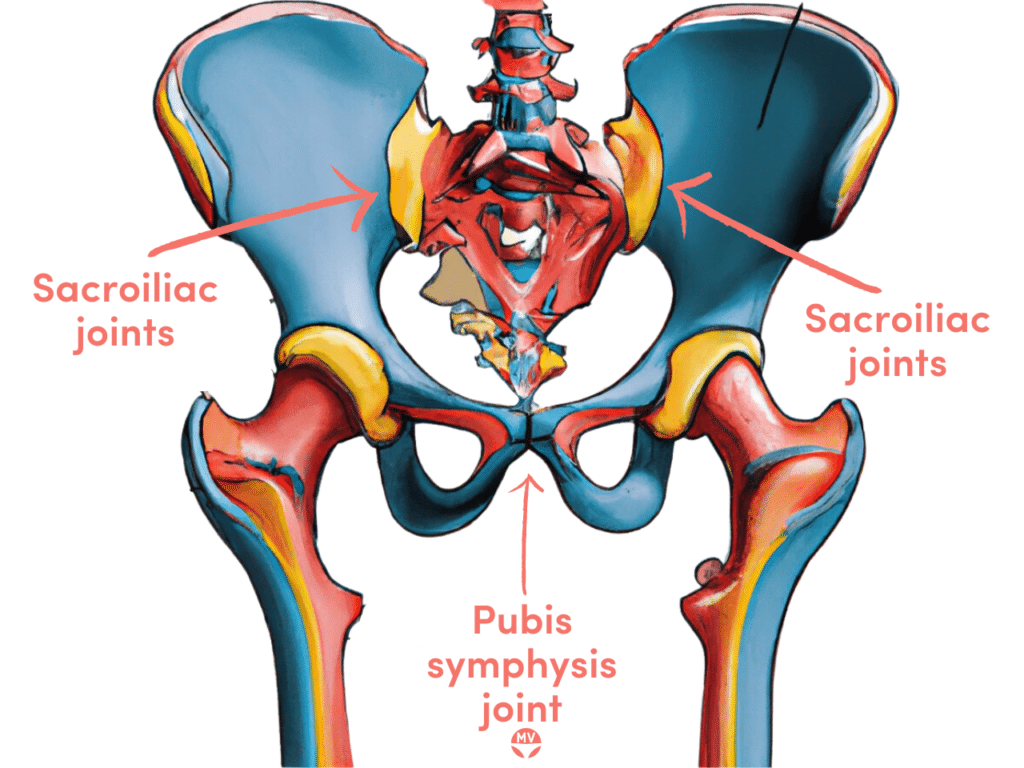
The symphysis pubis is a piece of cartilage connecting the front of the pelvic bone under the mons pubis. The sacroiliac joints and the pubis symphysis form a stable pelvic ring that, by design, doesn’t allow much mobility1.
Symphysis pubic dysfunction (SPD) is a term that may be used interchangeably during pregnancy with pelvic girdle pain (PGP), pelvic instability and lower back pain2, though these are not all the same issue.
Causes of SPD during pregnancy
A hormone called relaxin is released in a normal menstrual cycle, the first trimester of pregnancy, and again closer to the delivery date. Relaxin softens tissue, such as the uterus, blood vessels, cartilage and ligaments, to allow for the growth and stretching of tissue and then for a vaginal delivery.
This relaxing of cartilage can cause this very specific piece of pelvic cartilage – the symphysis pubis – to separate, resulting in excruciating pain.
Sometimes the relaxin surge occurs earlier, at around 20 weeks, causing many weeks of pain before delivery. In a first pregnancy, up to 60 per cent will experience symphysis pubis dysfunction (SPD) or a pelvic separation.
Symptoms of symphysis pubis dysfunction
- Stabbing pain in the groin area
- Excruciating hip, groin, glute and pubic area pain
- Wrenching pain when walking
- Feeling that the pelvis is cracking
- A sense that hips are dislocated or will dislocate
- Pain on walking, climbing stairs, rolling over in bed
How to manage SPD during pregnancy
The symphysis pubis will remain relaxed until the baby is born, so pain management is the only realistic option. One of the most effective ways to manage the pain is to use massage to release the muscles connected to the pelvis. A specific abdominal massage is Mayan abdominal massage, but there are many forms.
The attached pelvic muscles contain many nerve endings related to SPD pain, so relaxing these muscles can help reduce pain. Pain can be reduced by significant levels (up to 80 per cent) in just one visit to a pelvic physiotherapist or specialist, so make regular appointments, with 1-2 initially to reduce the majority of the pain, with follow-ups as needed.
The massage for SPD typically involves firm, deep massage techniques along the upper thighs, hips, glutes, groin and lower back. Massage has a three-fold effect of relaxing muscles, releasing endorphins, our natural painkillers, and increasing blood flow to the area. Most people find significant relief quickly.
At-home care can include gentle stretching of the lower back, glutes, hips and quads, but ask your therapist for advice and techniques. A support belt or special tape (KT/Roc) may be considered to reduce pressure.
Acupressure, reflexology and acupuncture can also be very helpful in pain management.
When SPD doesn’t go away after birth
Ligaments that surround and bridge the pubic symphysis joint can be damaged during pregnancy when relaxin levels are highest. Trauma or ‘shearing’ of the joint can occur from repetitive movements, slips or accidents that stress the looser joint and ligaments.
Ligaments are supposed to strengthen again after relaxin levels normalise, but weakness may remain for some. This continued weakness results in ongoing separation or shearing in the symphysis ligaments at the attachment sites. This continued shearing can cause lesions on the bones and cartilage, with pain that can take months or years to resolve.
What is relaxin?
Relaxin is an important reproductive hormone produced during a normal menstrual cycle, particularly during pregnancy. Relaxin relaxes the uterus, prepares the uterine lining for implantation, and prevents uterine contractions.
If conception doesn’t occur, relaxin decreases until the next menstrual cycle. If conception occurs, relaxin levels stay high and rise during the first trimester to help the body accommodate the growing foetus.
Once pregnant, the placenta also produces relaxin, with peak levels at 12-14 weeks. Over the coming weeks, relaxin levels will start to decline, with a surge closer to the delivery date. This extra relaxin can make you more susceptible to injury and may also cause pregnancy-related digestive issues like constipation.
References3–8
- 1.Kordi R, Abolhasani M, Rostami M, Hantoushzadeh S, Mansournia MA, Vasheghani-Farahani F. Comparison between the effect of lumbopelvic belt and home based pelvic stabilizing exercise on pregnant women with pelvic girdle pain; a randomized controlled trial. BMR. Published online April 29, 2013:133-139. doi:10.3233/bmr-2012-00357
- 2.Walters C, West S, Nippita TA. Pelvic girdle pain in pregnancy. Aust J Gen Pract. Published online July 1, 2018:439-443. doi:10.31128/ajgp-01-18-4467
- 3.RE L, D M, SW L. Symphysis pubis dysfunction: a review of the literature. Journal of Maternal-Fetal and Neonatal Medicine. Published online December 1, 2004:349-354. doi:10.1080/14767050400018247
- 4.Maclennan AH, Maclennan SC, The Norwegian Association for Women. Symptom-giving pelvic girdle relaxation of pregnancy, postnatal pelvic joint syndrome and developmental dysplasia of the hip. Acta Obstet Gynecol Scand. Published online January 1997:760-764. doi:10.3109/00016349709024343
- 5.Jain S, Eedarapalli P, Jamjute P, Sawdy R. Symphysis pubis dysfunction: a practical approach to management. The Obstetrician & Gynaecologist. Published online July 2006:153-158. doi:10.1576/toag.8.3.153.27250
- 6.Aslan E, Fynes M. Symphysial pelvic dysfunction. Current Opinion in Obstetrics & Gynecology. Published online April 2007:133-139. doi:10.1097/gco.0b013e328034f138
- 7.Owens K, Pearson A, Mason G. Symphysis pubis dysfunction—a cause of significant obstetric morbidity. European Journal of Obstetrics & Gynecology and Reproductive Biology. Published online November 2002:143-146. doi:10.1016/s0301-2115(02)00192-6
- 8.Howell E. Pregnancy-related symphysis pubis dysfunction management and postpartum rehabilitation: two case reports. J Can Chiropr Assoc. 2012;56(2):102-111. https://www.ncbi.nlm.nih.gov/pubmed/22675223






