A healthy microbiome can take many shapes and forms. There is a lot of variation in what is ‘healthy’ for each person when it comes to which bacteria and yeasts live in the vagina.
What is the vaginal microbiome?
The vaginal microbiome is a community of microbes – bacteria and yeasts/fungi – that live complex, interconnected lives inside the vagina. It’s also called vaginal flora or vaginal microbiota. The vaginal microbiome plays a major role in reproductive and vaginal health.
One of the main reasons women seek health advice is due to uncomfortable vaginal symptoms1. Over 90 per cent of these visits are due to an imbalanced vaginal microbiome2. These imbalances may include conditions such as bacterial vaginosis (BV), aerobic vaginitis (AV), yeast infections, cytolytic vaginosis (CV) and others.
The vaginal microbiome impacts more than just the vagina – imbalances are associated with complications during pregnancy, infertility, sexually transmitted infections (STIs) and sometimes even cancer3.
So why do we still know so little about the vaginal microbiome if it’s so important? Microbiology and study into the human microbiome is a quickly developing field, with most of the studies so far being on the gut and skin.
The gender healthcare gap means women and people with vaginas have been left out of research for the most part (but we’re helping fix that!).
Meet the players in the vaginal microbiome
The vaginal microbial community is composed of a diverse array of bacteria, fungi, viruses, and other organisms. The main standout player in most healthy vaginas is Lactobacillus species, our ‘friendly’ or ‘good’ bacteria.
Enter stage left, lactobacilli
Lactobacilli are pretty handy to have around because they produce lactic acid to keep the vaginal pH between 3.8 and 4.5. Lactic acid is harmful to most other bacteria, so they stay away.
Lactobacilli use up vaginal real estate, living on vaginal cells, keeping the cells protected from other bacteria moving in. Lactobacilli also produce bacteriocins – a natural antibiotic – to keep harmful bacteria populations down.
Lactobacilli also keep inflammation down.
Three of our favourite lactobacilli species are Lactobacillus crispatus, L. jensenii and L. gasseri.
Meet the creeps – disruptive vaginal microbes
If your lactobacilli friends are in short supply, other bacteria that are not so helpful will take their place. These potentially disruptive microbes include Gardnerella, Ureaplasma, yeast like Candida, or even E. coli and other bacteria that belong in the digestive system.
When there are too many unfriendly bacteria in the vagina, we call this vaginal dysbiosis4. Put simply, it just means ‘bacteria out of balance’ or ‘too many of the wrong bugs in the wrong place’, which is different to, say, a vaginal infection. Vaginal dysbiosis and vaginal infections are not the same thing.
Bacterial vaginosis (BV) is the most common form of vaginal dysbiosis. Each year, about 1 in 3 women will develop BV5. Some groups of women are affected more than others6. Other forms of vaginal dysbiosis include yeast infections (thrush), urinary tract infections (UTIs) and aerobic vaginitis (AV), and can cause itching, burning, unpleasant odours and irritation.
But not everyone gets symptoms, and not everyone needs treatment. A healthy vaginal microbiome is one that doesn’t cause problems for you or your sexual partners.
Unfortunately, misdiagnosis rates are high, as are recurrence rates after conventional treatments – over 50% of cases of BV recur after antibiotic treatment.
Here at My Vagina, we are diving into the how and why of these recurrences, working on treatments that address the underlying drivers of vaginal dysbiosis, not just the microbiome disturbances. We are doing unique research into the driving factors that influence the vaginal microbiome.
Understanding the driving forces behind vaginal microbiome issues means treating the cause, not just the microbes or symptoms. As anyone with recurring vaginal symptoms will know, antibiotics and probiotics can only take you so far.
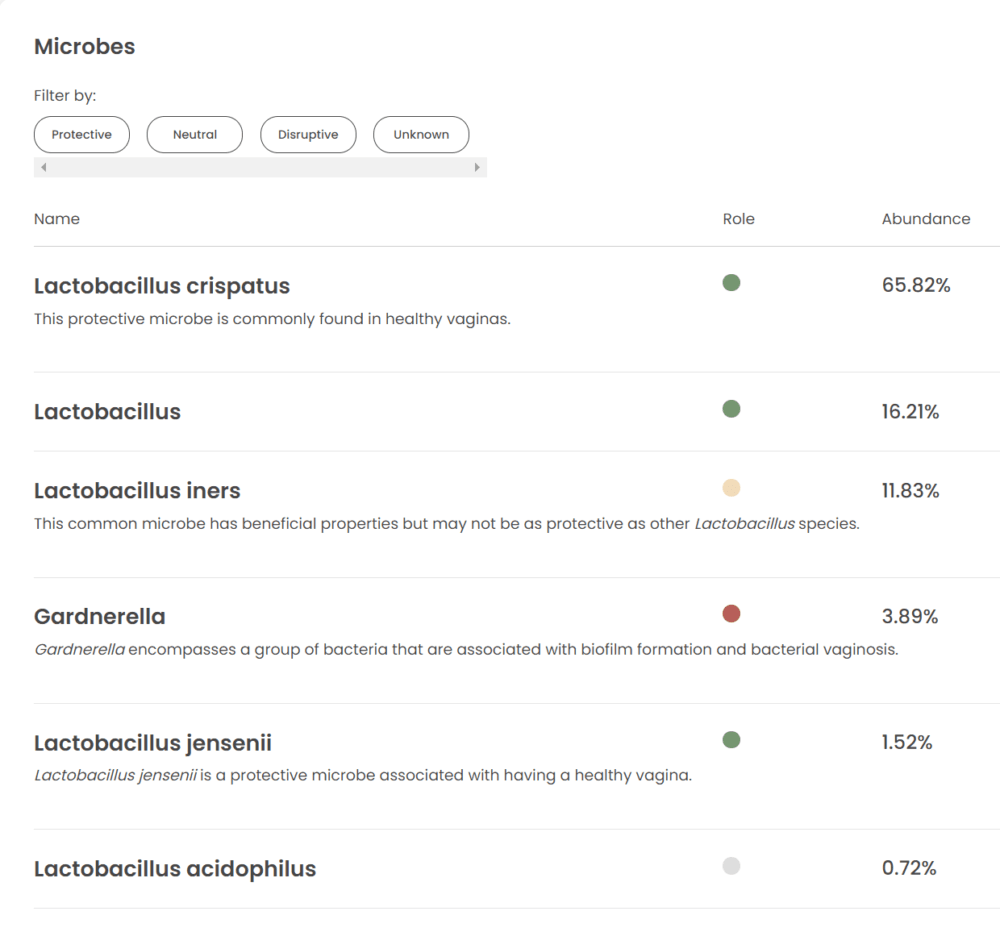
What a protective vaginal microbiome looks like
Your test doesn’t have to come back ‘perfect’ to be great! It’s a good sign to have a small range of bacteria present, with the majority protective species.
Below is a good-looking vaginal microbiome tested using Juno, from the vagina of someone not experiencing vaginal symptoms.
Testing the vaginal microbiome at home
If you don’t have symptoms, your vaginal microbiome may be just fine for you. If you have symptoms, getting a comprehensive vaginal microbiome test is a great idea, no doctor required. Order online anywhere in the world.
How vaginal flora impacts the rest of your body
When vaginal flora is disrupted, it allows disruptive bacteria and fungi to move in, which can lead to inflammation of vaginal cells. Many pathogens can interfere with vaginal cells’ ability to defend themselves, blocking the immune response.
With a strong colony of lactobacilli in the vagina, disruptors are kept at bay, maintaining vaginal immunity and defence systems.
Some broader impacts of vaginal microbiome disturbances include being at greater risk of catching an STI7, pelvic inflammatory disease (PID)8, infertility9 or failures of IVF treatments10, miscarriage11, premature babies12, preeclampsia13 and problems in newborn babies14. Other serious health problems include certain gynaecological cancers (ovarian15, cervical16, endometrial17).
Vaginal flora changes with your body
The microbes in your vagina change all the time depending on the menstrual cycle (or lack of), sex, changing hormones (pregnancy, birth control, post-partum, menopause18), and behaviours like smoking19, stress20, douching and certain medications.
Understanding Community State Types (CSTs)
You might see on some vaginal microbiome reports a Community State Type listed. This is a broad classification of which lactobacilli species dominate the vagina, or, in the case of CST Type 4, are not dominated by lactobacilli.
- Type 1: Lactobacillus crispatus
- Type 2: Lactobacillus gasseri
- Type 3: Lactobacillus iners
- Type 4: Non-lactobacilli species dominant, five subgroups
- Type 5: Lactobacillus jensenii
Generally speaking, CSTs 1, 2 and 5 are considered more favourable, but take this information as a broad sweeping generalisation only.
References
- 1.Kairys N, Garg M. Bacterial Vaginosis. . National Library of Medicine. Published 2023. https://www.ncbi.nlm.nih.gov/books/NBK459216/
- 2.Sobel JD. Vaginal Infections in Adult Women. Medical Clinics of North America. Published online November 1990:1573-1602. doi:10.1016/s0025-7125(16)30496-5
- 3.Champer M, Wong A, Champer J, et al. The role of the vaginal microbiome in gynaecological cancer. BJOG. Published online April 12, 2017:309-315. doi:10.1111/1471-0528.14631
- 4.van de Wijgert JHHM, Jespers V. The global health impact of vaginal dysbiosis. Research in Microbiology. Published online November 2017:859-864. doi:10.1016/j.resmic.2017.02.003
- 5.Koumans EH, Sternberg M, Bruce C, et al. The Prevalence of Bacterial Vaginosis in the United States, 2001–2004; Associations With Symptoms, Sexual Behaviors, and Reproductive Health. Sexually Transmitted Diseases. Published online November 2007:864-869. doi:10.1097/olq.0b013e318074e565
- 6.Ravel J, Gajer P, Abdo Z, et al. Vaginal microbiome of reproductive-age women. Proc Natl Acad Sci USA. Published online June 3, 2010:4680-4687. doi:10.1073/pnas.1002611107
- 7.Brotman RM. Vaginal microbiome and sexually transmitted infections: an epidemiologic perspective. J Clin Invest. Published online December 1, 2011:4610-4617. doi:10.1172/jci57172
- 8.Haggerty CL, Totten PA, Tang G, et al. Identification of novel microbes associated with pelvic inflammatory disease and infertility. Sex Transm Infect. Published online January 29, 2016:441-446. doi:10.1136/sextrans-2015-052285
- 9.van Oostrum N, De Sutter P, Meys J, Verstraelen H. Risks associated with bacterial vaginosis in infertility patients: a systematic review and meta-analysis. Human Reproduction. Published online March 29, 2013:1809-1815. doi:10.1093/humrep/det096
- 10.Skafte-Holm A, Humaidan P, Bernabeu A, Lledo B, Jensen JS, Haahr T. The Association between Vaginal Dysbiosis and Reproductive Outcomes in Sub-Fertile Women Undergoing IVF-Treatment: A Systematic PRISMA Review and Meta-Analysis. Pathogens. Published online March 4, 2021:295. doi:10.3390/pathogens10030295
- 11.Leitich H, Kiss H. Asymptomatic bacterial vaginosis and intermediate flora as risk factors for adverse pregnancy outcome. Best Practice & Research Clinical Obstetrics & Gynaecology. Published online June 2007:375-390. doi:10.1016/j.bpobgyn.2006.12.005
- 12.Kosti I, Lyalina S, Pollard KS, Butte AJ, Sirota M. Meta-Analysis of Vaginal Microbiome Data Provides New Insights Into Preterm Birth. Front Microbiol. Published online April 8, 2020. doi:10.3389/fmicb.2020.00476
- 13.Lin CY, Lin CY, Yeh YM, et al. Severe preeclampsia is associated with a higher relative abundance of Prevotella bivia in the vaginal microbiota. Sci Rep. Published online October 26, 2020. doi:10.1038/s41598-020-75534-3
- 14.Dingens AS, Fairfortune TS, Reed S, Mitchell C. Bacterial vaginosis and adverse outcomes among full-term infants: a cohort study. BMC Pregnancy Childbirth. Published online September 22, 2016. doi:10.1186/s12884-016-1073-y
- 15.Nené NR, Reisel D, Leimbach A, et al. Association between the cervicovaginal microbiome, BRCA1 mutation status, and risk of ovarian cancer: a case-control study. The Lancet Oncology. Published online August 2019:1171-1182. doi:10.1016/s1470-2045(19)30340-7
- 16.Yang X, Da M, Zhang W, Qi Q, Zhang C, Han S. Role of <em>Lactobacillus</em> in cervical cancer. CMAR. Published online May 2018:1219-1229. doi:10.2147/cmar.s165228
- 17.Walther-António MRS, Chen J, Multinu F, et al. Potential contribution of the uterine microbiome in the development of endometrial cancer. Genome Med. Published online November 25, 2016. doi:10.1186/s13073-016-0368-y
- 18.Muhleisen AL, Herbst-Kralovetz MM. Menopause and the vaginal microbiome. Maturitas. Published online September 2016:42-50. doi:10.1016/j.maturitas.2016.05.015
- 19.Brotman RM, He X, Gajer P, et al. Association between cigarette smoking and the vaginal microbiota: a pilot study. BMC Infect Dis. Published online August 28, 2014. doi:10.1186/1471-2334-14-471
- 20.Witkin S, Linhares I. Why do lactobacilli dominate the human vaginal microbiota? BJOG. Published online November 7, 2016:606-611. doi:10.1111/1471-0528.14390