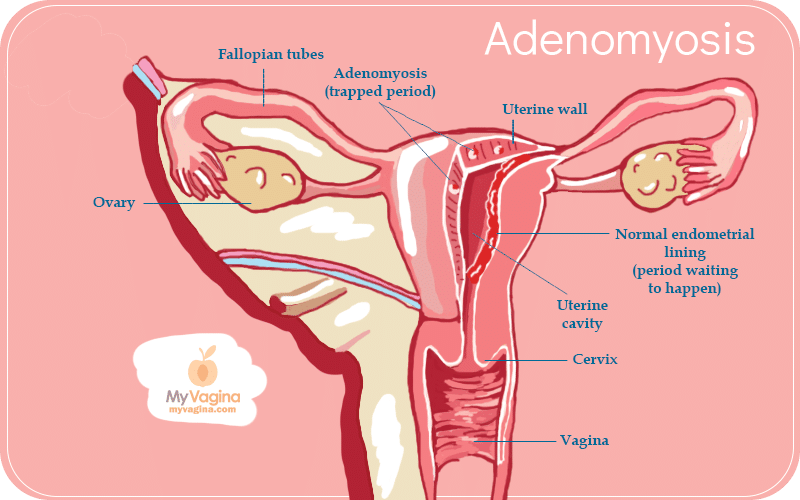
Endometrial adenomyosis is a condition whereby endometrial tissue (the cells that produce period blood) are found inside the uterine wall instead of just on it.
The endometrial tissue grows in the wrong area but behaves as it would normally – growing, thickening, then dispersing and bleeding, as a period does.
Adenomyosis is very painful, causing inflammation, swelling, and abnormal uterine bleeding (AUB). While most people diagnosed with adenomyosis are aged 40-50 and have had pregnancies, it’s becoming clear that this condition is present in younger people who have never been pregnant but may go undiagnosed.
Younger people with unexplained severe pain, AUB, infertility or no symptoms (identified by transvaginal ultrasound or MRI) are increasingly being diagnosed, challenging the diagnostic boundaries.
Adenomyosis is considered a benign endometrial condition, which means it’s not a condition that threatens life or body, like cancer. But, anyone with this painful condition will tell you it seriously threatens a happy life.
Diagnosis of adenomyosis
Diagnosis is typically made after removal of the uterus by hysterectomy, where the diagnosis can be confirmed. New techniques in imaging can be useful, including ultrasound and magnetic resonance imaging (MRI). 1
There isn’t agreement on the classification or definition of adenomyotic lesions in histopathology or imaging perspectives, making the diagnosis difficult and murky. There is no single theory to offer an explanation for the differing presentations of adenomyosis.
Adenomyosis usually appears in clinical practice with other gynaecological conditions such as fibroids and endometriosis. Treatment is a lifelong management plan to improve quality of life, fertility, pregnancy outcomes and menstrual symptoms. There is a high risk of miscarriage and other pregnancy complications. 2,3
Symptoms of endometrial adenomyosis
There is usually no sign of adenomyosis until after childbearing but before menopause, and it disappears by itself after menopause in most cases, which points to hormonal links, in particular the influence of oestrogen. Adenomyosis can also have no symptoms or mild symptoms. 4
- Heavy or long periods (menorrhagia)
- Severe painful cramping and pelvic pain during menstruation (secondary dysmenorrhoea)
- Cramps for the entire menstrual period, instead of just the start
- Clots
- Pain during sex (dyspareunia)
- Enlarged, tender abdomen
Causes of endometrial adenomyosis
The specific cause of adenomyosis isn’t known. The symptoms don’t exist after menopause, as menstrual bleeding stops; thus, the cause of the pain and symptoms is removed. Adenomyosis seems to be directly affected by oestrogen, with another trigger being surgery of some kind.
Adenomyosis remains a bit of a mystery to medicine, but further research continues. 5
Risk factors of endometrial adenomyosis
Risk factors include caesareans or other surgeries (such as removing fibroids) on the uterus, where the endometrial tissue can be misplaced in the uterine lining.
There appears to be a link between childbirth and adenomyosis, with the inflammation of the uterus after birth possibly resulting in a small break in the lining, allowing endometrial cells to enter, which then closes up and heals, causing the cells to be stuck there.
Theories include that endometrial cells are mistakenly placed into the uterine muscle during development as a foetus and stem cell invasion.
Secondary problems
Heavy bleeding can result in anaemia, with fatigue and an impact on all body systems. This condition can be very painful and cause major disruptions to your life.
Pain increases the intake of medications which also have secondary impacts on body functioning, and pain can stop you from being able to go about normal daily activities, including work and school.
Chronic pain conditions also increase the likelihood of depression, anxiety, mood disorders, and a feeling of a lack of control over one’s life and body.
Treatment of endometrial adenomyosis
To start with, you will see your doctor or gynaecological specialist, who will evaluate your signs and symptoms with questions and a pelvic examination.
An ultrasound or MRI will help properly diagnose your condition, eliminating other causes of symptoms. A biopsy may be taken. 6
At this point, the main medical treatment for severe adenomyosis is a hysterectomy, though this is improving in terms of options.7 Manipulating hormones can also be a very useful management tool.
Managing endometrial adenomyosis symptoms
- Anti-inflammatory drugs to reduce the pain – usually prescribed to those nearing menopause, since ‘it’s nearly over anyway’
- Hormone therapy – birth control pills may be prescribed to manage hormone levels and lessen bleeding and pain
- Some contraceptives (including IUDs and the oral contraceptive pill) can completely stop menstrual bleeding, eliminating much of the pain and suffering
- Heat pads or packs on the abdomen
Keep in mind that the only real way to test for adenomyosis is to remove the entire uterus (hysterectomy) and check. This is branching on hysteria if your symptoms do not warrant such a drastic move, and other measures will be taken to try to avoid this step if possible.
It is also probably going to take a while to be diagnosed with adenomyosis, using a process of elimination of many other conditions that may cause the same symptoms, including (but not limited to) cancer, fibroids, endometriosis or polyps.
Adenomyosis may be the last diagnosis after the other avenues have been exhausted. This process can be really stressful, but eliminating other options is important.
Endometrial adenomyosis support
Support options for endometrial adenomyosis range from maintaining healthy hormone levels to dealing with the impacts of conventional treatments.
The recommendations made by your primary care physician will be discussed with you. Once you have a firm diagnosis, managing symptoms and hormones can become important.
Oestrogen excess and clearance
Non-drug treatments to normalise hormones are available, which may include reducing oestrogen excess.
Diet changes can fast-track oestrogen clearance through the bowel by increasing fibre intake, for example, or adjusting food choices.
Exercise and liver support can also improve oestrogen clearance. Treatments may also include pressure point therapies like acupuncture or reflexology.
Pressure point therapies can help manage and relieve pain temporarily, used as an ongoing pain-relieving/management strategy.
Having other practitioners besides your regular doctor providing support for adenomyosis can mean you get a range of views on your condition, and more than one way to help yourself.
There are many strategies to alleviate pain or modify the body’s behaviour in positive ways. You may find relief in mindfulness and meditation techniques all the way to yoga, osteopathy, traditional Chinese medicine, naturopathy, herbalism and other supportive, complementary approaches.
It’s always important to inform each of your practitioners of everything you are taking to ensure safety – not all drugs and herbs, or other treatments, are always safe to use with one another or with certain health conditions.
Never assume that herbs or supplements are safe just because they are ‘natural’. Natural does not mean safe.
Getting help with adenomyosis symptoms
If you have a diagnosis of adenomyosis and want support, speak to a specialist practitioner alongside your doctor.
References8
- 1.Moawad G, Fruscalzo A, Youssef Y, et al. Adenomyosis: An Updated Review on Diagnosis and Classification. JCM. Published online July 21, 2023:4828. doi:10.3390/jcm12144828
- 2.Schrager S, Yogendran L, Marquez C, Sadowski E. Adenomyosis: Diagnosis and Management. Am Fam Physician. 2022;105(1):33-38. https://www.ncbi.nlm.nih.gov/pubmed/35029928
- 3.Mishra I, Melo P, Easter C, Sephton V, Dhillon‐Smith R, Coomarasamy A. Prevalence of adenomyosis in women with subfertility: systematic review and meta‐analysis. Ultrasound in Obstet & Gyne. Published online April 28, 2023:23-41. doi:10.1002/uog.26159
- 4.Gordts S, Grimbizis G, Campo R. Symptoms and classification of uterine adenomyosis, including the place of hysteroscopy in diagnosis. Fertility and Sterility. Published online March 2018:380-388.e1. doi:10.1016/j.fertnstert.2018.01.006
- 5.Guo SW. Cracking the enigma of adenomyosis: an update on its pathogenesis and pathophysiology. Reproduction. Published online November 1, 2022:R101-R121. doi:10.1530/rep-22-0224
- 6.Moawad G, Youssef Y, Fruscalzo A, et al. The Present and the Future of Medical Therapies for Adenomyosis: A Narrative Review. JCM. Published online September 22, 2023:6130. doi:10.3390/jcm12196130
- 7.Taran F, Stewart E, Brucker S. Adenomyosis: Epidemiology, Risk Factors, Clinical Phenotype and Surgical and Interventional Alternatives to Hysterectomy. Geburtsh Frauenheilk. Published online October 11, 2013:924-931. doi:10.1055/s-0033-1350840
- 8.Vannuccini S, Petraglia F. Recent advances in understanding and managing adenomyosis. F1000Res. Published online March 13, 2019:283. doi:10.12688/f1000research.17242.1