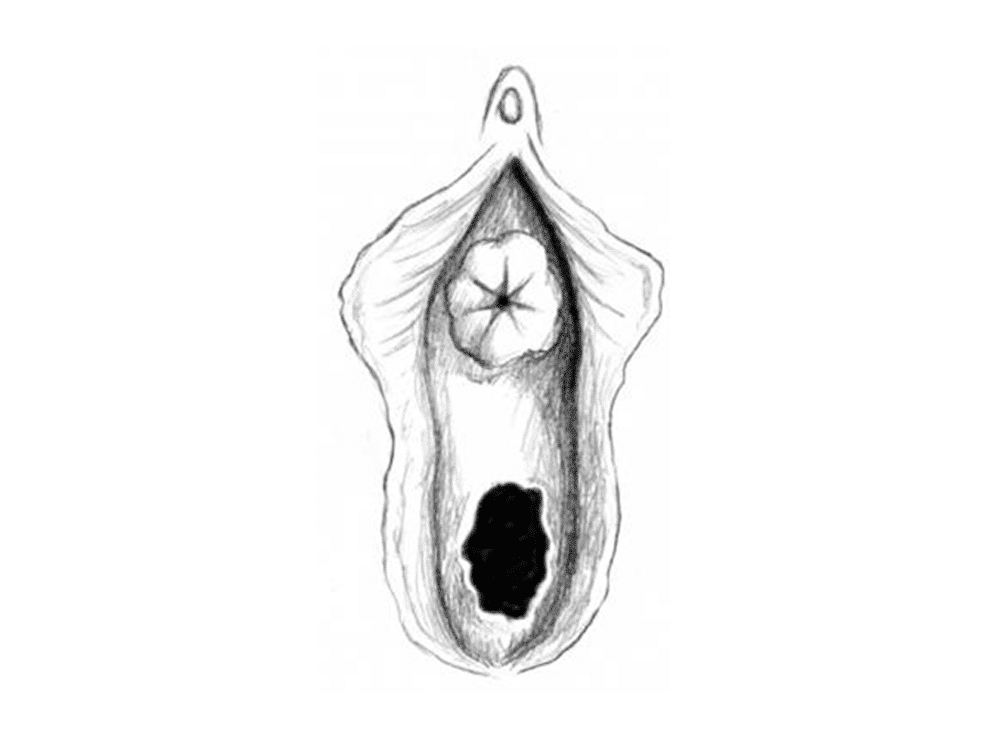
Urethral prolapse is a condition whereby the outer end of the urethra protrudes from its exit point on the vulva (the urinary meatus).
Urethral prolapse is an uncommon condition that seems to mostly affect girls of African descent prior to puberty (under age 10) and postmenopausal Caucasian women.
There is a more advanced and even rarer version of urethral prolapse called a strangulated urethral prolapse. Because of its rarity, urethral prolapse misdiagnosis rates are high.
Symptoms of a urethral prolapse
- No symptoms may be present, particularly in young girls
- Adult women are usually symptomatic
- Bleeding or spotting in underwear or diaper/nappy
- Protrusion visible from urethral opening upon examination
- Problems urinating – increased frequency, pain, burning, waking up in the night to urinate
- Urinary tract infections
Treatments for urethral prolapse
Historically, treatment for a urethral prolapse was usually surgical, however new, effective, non-surgical treatments include topical oestrogen cream or other topical ointments.
The oestrogen cream strengthens the tissue so it stays where it is supposed to. Prolapse means that the tissue falls out of place, in this case because for some reason it is weaker than it ought to be.
Non-surgical treatments for urethral prolapse
- Sitz baths
- Topical antibiotics
- Steroid creams
- In children, oestrogen cream is applied to the prolapsed urethra 2-3 times per day for two weeks along with sitz baths
- In women, oral conjugated oestrogen may be given for mild prolapse, or topical oestrogen cream applied 2-3 times per day for 2 weeks, with sitz baths
Failure of non-surgical urethral prolapse treatments results in the consideration of surgery. In severe cases, surgery may be recommended immediately if tissue is severely damaged
Urethral prolapse surgery
Strangulated urethral prolapse usually requires surgery. The surgery for urethral prolapse and strangulated urethral prolapse varies depending on the individual and the surgeon, with a solid success rate.
Older surgical procedures are not performed anymore, with newer procedures more effective and safer.
Urethral prolapse surgery includes realigning the two layers of smooth muscle that make up the urethra, or removing the protruding end.
Oestrogen cream is usually applied as well, and a catheter may be used for a short time as the urethra heals. There may be some rare complications to surgery.
Note: women who have had oestrogen-dependent breast cancers won’t be prescribed oestrogen creams. Please see the atrophic vaginitis article for women on post-breast-cancer hormone-blocking therapies.
Note: urethral prolapse is different from a urethral caruncle, which is a condition where about a quarter of the urethral tissue protrudes from the body.
Who gets urethral prolapse
The distribution of age is very marked, with girls under 10 and postmenopausal women. An interesting point is a pair of identical twins both got urethral prolapse, suggesting a hereditary influence.
Girls under 10 may develop urethral prolapse, with average onset age four years. Postmenopausal women are the next group to experience urethral prolapse, though it can affect any woman.
Frequently prescribed hormone therapy (oestrogen) post menopause has reduced the incidence of urethral prolapse in postmenopausal women. Both these groups have little or no oestrogen in their bodies.
Oestrogen is known to exert an influence on skin integrity, meaning the lack of oestrogen can affect tissues in a negative way, allowing easier damage and irregularities like a urethral prolapse.
Strangulated urethral prolapse is more common in adults than children. Urethral prolapse does not generally affect men.
Causes of urethral prolapse
The cause of urethral prolapse is as yet unknown, however there are some theories. General pelvic tissue weakness contributes.
Congenital birth defects
Congenital defects are abnormalities that we are born with. These abnormalities may include weak pelvic floor muscles, which are the structures that support everything in the pelvis.
Abnormalities in a developing foetus can result in pelvic attachments not being fully formed or properly functioning, and this can allow the urethra to move around more than it normally should.
The causes of abnormalities in a foetus can vary. Suggestions include neuromuscular disorders, poor urethral positioning, and deficiencies in the elasticity of the tissue.
An acquired defect
An acquired defect is an issue that alters function or appearance after or during birth, including sexual abuse, masturbation, malnutrition and debility.
There may be a weak attachment between smooth muscle layers of the urethra. This weak attachment may predispose someone to urethral prolapse after perhaps a lot of coughing or constipation (intra-abdominal pressure).
How urethral prolapse works
There are two layers of smooth muscle that make up the urethra – the inner and outer layers. In a healthy urethra, these two layers are firmly adhered together.
If the two layers separate for some reason, one of the layers can slide out the opening, since it is no longer attached to the other. If this prolapse is not treated, the resultant swelling can cut off the blood supply to the protruding piece of urethra, causing the tissue to die.
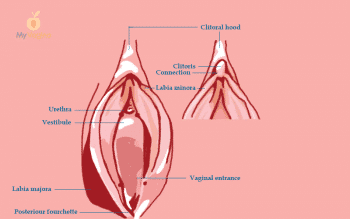
Anatomy of the urethra
The urethra is about 4 cm long in an adult woman, and runs from the neck of the bladder to the external urinary meatus, which is the exit area of urine, between the labia, above the vaginal opening, and below the clitoris.
The urethra is made up of mucosal tissue, with secretory glands lining the walls to provide lubrication. These periurethral glands are actually the Skene glands, which empty out of two small ducts on either side of the meatus.
The tissue surrounding the urethra (mucosa and submucosa) offer some level of bladder control via the mucosal seal. All the mucosa in the urethral tissue is very sensitive to oestrogen, so a low level of oestrogen can result in the tissue becoming weak and atrophying, loosening the mucosal seal and allowing incontinence.
Contraction and relaxation of one of the smooth muscle layers allows the urethra to shorten and widen to allow urination.
Can urethral prolapse be treated with natural medicine?
All prolapse needs to be carefully investigated by a physician to determine causality and provide an accurate diagnosis.
The aim of treatment is the same in conventional and natural medicine: to strengthen urethral tissue so it stays in place on its own.
An integrative approach often provides the best outcomes for patients with urethral prolapse, with conventional and natural medicine practices all having a beneficial role.
The most comprehensive vaginal microbiome test you can take at home, brought to you by world-leading vaginal microbiome scientists at Juno Bio.
Unique, comprehensive BV, AV and 'mystery bad vag' treatment guide, one-of-a-kind system, with effective, innovative treatments.
Promote and support a protective vaginal microbiome with tailored probiotic species.