Aerobic vaginitis (AV) is an inflammatory vaginal microbial condition. Aerobic means the bacteria that dominate the vaginal flora prefer to live in an environment with oxygen, while vaginitis means vaginal inflammation.
The name ‘aerobic’ is somewhat misleading, as many AV-related bacteria can survive in anaerobic (oxygen-free) conditions, a characteristic known as facultative.
AV can cause symptoms and comes with complications such as preterm labour, increased risk of contracting sexually transmitted infections, and abnormal Pap test results.
AV may be confused with bacterial vaginosis (BV) without proper testing.
Symptoms of aerobic vaginitis
- Yellowish/greenish discharge
- Thick, sticky or irritating discharge
- Rotten, foul odour, faeces, rotten meat, dead smell
- Inflammation of the vagina and/or vulva
- Symptoms improve during menstrual bleeding
- Redness
- Itching
- Soreness
- Possibly ulcers or erosions
- Burning or stinging sensation
- Swelling
- Painful sex (dyspareunia)
- pH may be 4.0+ (so not always a good indicator) (test vaginal pH at home)
- Signs of atrophy on vaginal cells
- Possibly long-lasting symptoms after multiple unsuccessful treatments
- May be asymptomatic
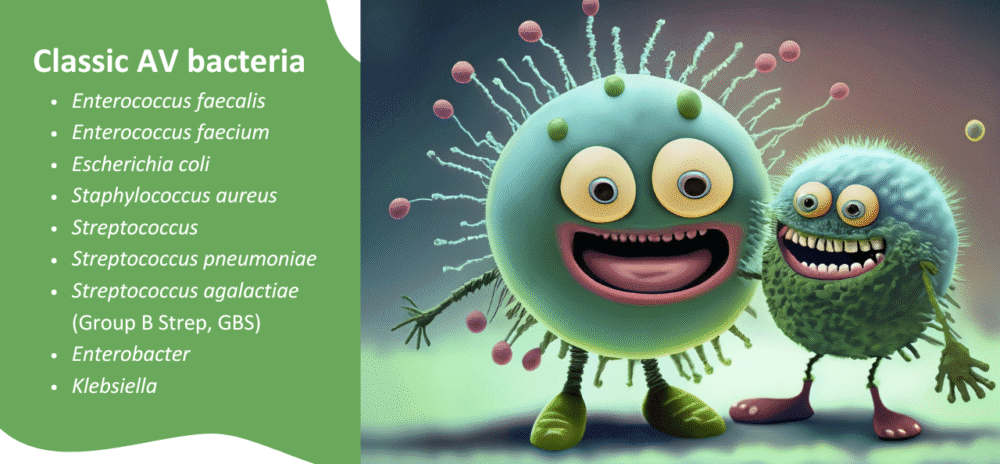
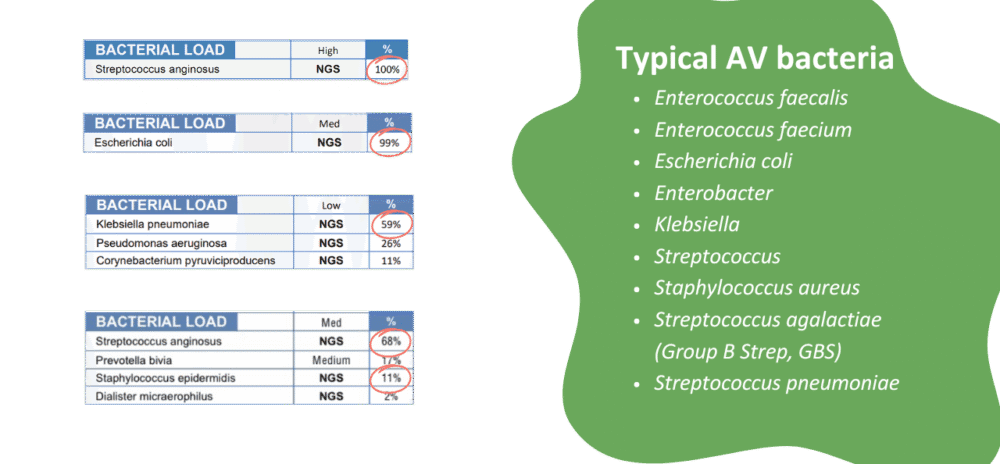
Most common AV-causing bacteria
The most common causes of AV are E. coli, E. faecalis, and Group B Strep.
- Escherichia coli
- Enterococcus faecalis
- Group B Strep (GBS) Streptococcus agalactiae
- Staphylococcus aureus
- Staphylococcus epidermidis
- Klebsiella
Treatment for aerobic vaginitis
Several conventional and non-drug treatments are available to treat AV. It might be important, however, to consider the greater systemic environment if AV and UTIs are recurrent/chronic.
You can find significant information and treatment recommendations for AV in Killing BV. If symptoms are non-responsive to treatment, book with a My Vagina practitioner. We understand the drivers of AV and UTIs better than most practitioners and can provide valuable assistance.
My Vagina’s non-drug treatments for AV
My Vagina’s natural treatments for AV are powerful herbal medicines that target AV-causing bacteria specifically. The AV Vaginal Pessary does not contain any prebiotic lactulose, since lactulose contains fructose, an energy source for many AV-causing bacteria. Group B Strep is one such exception.
If you’re unsure, check the list of Bacteria that love lactulose.
Antibiotic treatment of aerobic vaginitis
Local (vaginal) antibiotics may be prescribed, often broad-spectrum, to cover both gram-positive and gram-negative aerobes (such as kanamycin). Oral antibiotic treatments with amoxiclav or moxifloxacin may be used, particularly if group B strep or methicillin-resistant Staphylococcus aureus (MRSA) is present.
Oral antibiotic use is discouraged in aerobic vaginitis, with topical treatments favoured by doctors due to their low absorbency and high concentrations where they matter.
Treatments should maximise the survival of lactobacillus species where possible, while effectively killing Gram-negative bacteria like E. coli, S. aureus, and E. faecalis. Combination treatment may be most appropriate due to antibiotic resistance, but your doctor will prescribe based on your circumstances and the latest drug recommendations.
Antibiotic vaginal gel and hydrocortisone suppositories may be effective in eradicating aerobic vaginitis. Some antibiotics are problematic and won’t work, and resistance is common in some countries. Talk to your doctor about their recommendations.
AV: Getting tested and treated
Knowing the specific bacteria in your vagina via a comprehensive vaginal microbiome test is useful for targeted treatment. Discuss a microbiome panel with your doctor about antibiotic sensitivities/resistance genes.
If treatments are consistently failing, book with one of our vulvovaginal specialist naturopathic practitioners for individualised care and practitioner-only treatments.
The relationship between AV and UTIs
AV-related bacteria are implicated in urinary tract infections (UTIs), and the bacteria can migrate back and forth between the vagina and urinary tract due to proximity or because a systemic energy source is plentiful.
In the case of frequent/chronic UTIs, just treating the vagina is unlikely to yield long-lasting results, but symptom management, as the UTI issue is resolved via other means, can be achieved.
AV can point to a greater systemic microbiome problem (gut, urinary tract, pathways) that may benefit from broader investigations and non-drug treatments.
Here at My Vagina’s specialist clinic, we’ve also noticed a relationship between AV and CV.
When AV turns into DIV
The most severe form of AV is called desquamative inflammatory vaginitis (DIV), but DIV may not be associated with bacteria or infection.
Understanding the gut microbiome in AV and chronic UTI
Treatment complexity can arise with AV and UTIs because bacteria may be commensal (normal, healthy) in other areas of the body, such as the digestive tract or mouth, but have colonised the vagina or urinary tract, causing symptoms.
There may be a larger body-wide imbalance occurring, so treating the vagina alone may be missing the true problem. Book with a My Vagina practitioner for support – we know what to do.
Diagnosis of aerobic vaginitis
Diagnosing aerobic vaginitis requires a positive test with the dominant strain in the vaginal microbiome being one or more of the AV-causing bacteria, alongside a loss of healthy lactobacillus species, and sometimes an elevated vaginal pH reading.
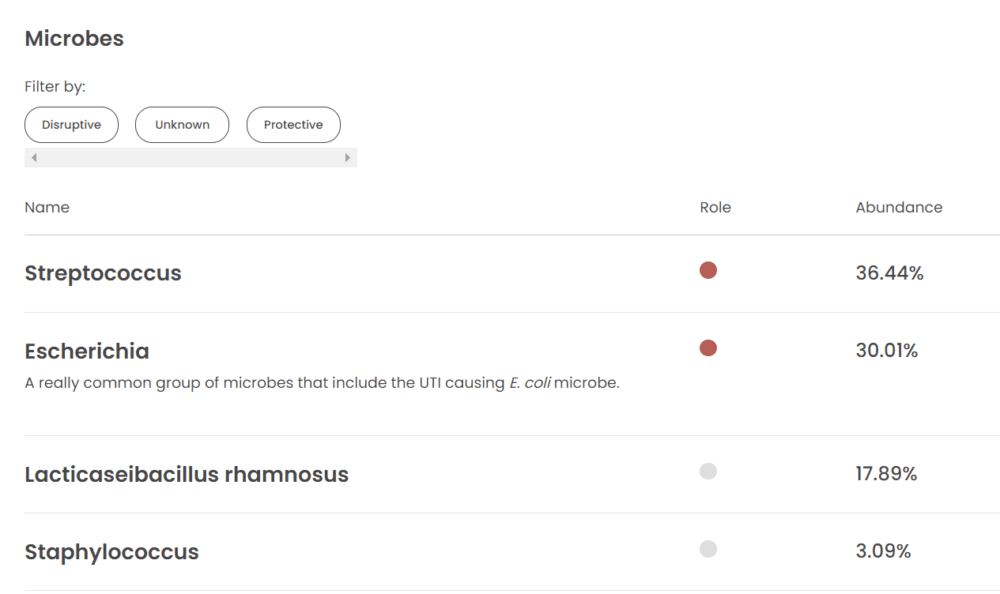
Get an accurate, comprehensive vaginal microbiome test
The most helpful test for determining the bacterial profile of your vagina is a comprehensive microbiome panel, which can be ordered by your practitioner or purchased online and completed at home.
These incredible vaginal microbiome tests provide a comprehensive view of the types and amounts of bacteria and fungi/yeast present in your vagina, as well as your microbial load and a snapshot of your pH.
How do I get an at-home AV test kit?
There are many emerging providers; however, here at My Vagina, we use Juno Bio. The tests are accurate, quick, and easy to read, and each test comes with a complimentary 15-minute coaching session from a Juno scientist. Additionally, Juno ships to most locations worldwide.
What to do with your vaginal microbiome results
Speak to the practitioner who ordered the test, if you have one. If you aren’t getting results, we can help.
My Vagina practitioners offer high-level microbiome analysis using a naturopathic lens. We know things nobody else knows about vaginas, having assessed thousands of results and spoken to each person they belong to.
Example of an AV vaginal microbiome (Juno Bio test)
Example of an AV vaginal microbiome (MicroGenDX tests)
Getting help for recurrent AV
Enrol in Killing BV and gain a deeper understanding of the problem so you can choose the next best steps.
Book with a My Vagina vulvovaginal specialist naturopath, or another practitioner who deeply understands the vaginal microbiome and can provide effective treatment.
References1–5
- 1.Donders GGG, Bellen G, Grinceviciene S, Ruban K, Vieira-Baptista P. Aerobic vaginitis: no longer a stranger. Research in Microbiology. Published online November 2017:845-858. doi:10.1016/j.resmic.2017.04.004
- 2.Casa V, Noll H, Gonser S, Grob P, Graf F, Pohlig G. Antimicrobial Activity of Dequalinium Chloride against Leading Germs of Vaginal Infections. Arzneimittelforschung. Published online December 26, 2011:699-705. doi:10.1055/s-0031-1299954
- 3.Jahic M, Mulavdic M, Nurkic J, Jahic E, Nurkic M. Clinical Characteristics of Aerobic Vaginitis and Its Association to Vaginal Candidiasis, Trichomonas Vaginitis and Bacterial Vaginosis. Med Arh. Published online 2013:428. doi:10.5455/medarh.2013.67.428-430
- 4.Donders GGG, Ruban K, Bellen G. Selecting Anti-Microbial Treatment of Aerobic Vaginitis. Curr Infect Dis Rep. Published online April 22, 2015. doi:10.1007/s11908-015-0477-6
- 5.Mendling W, Weissenbacher ER, Gerber S, Prasauskas V, Grob P. Use of locally delivered dequalinium chloride in the treatment of vaginal infections: a review. Arch Gynecol Obstet. Published online October 27, 2015:469-484. doi:10.1007/s00404-015-3914-8